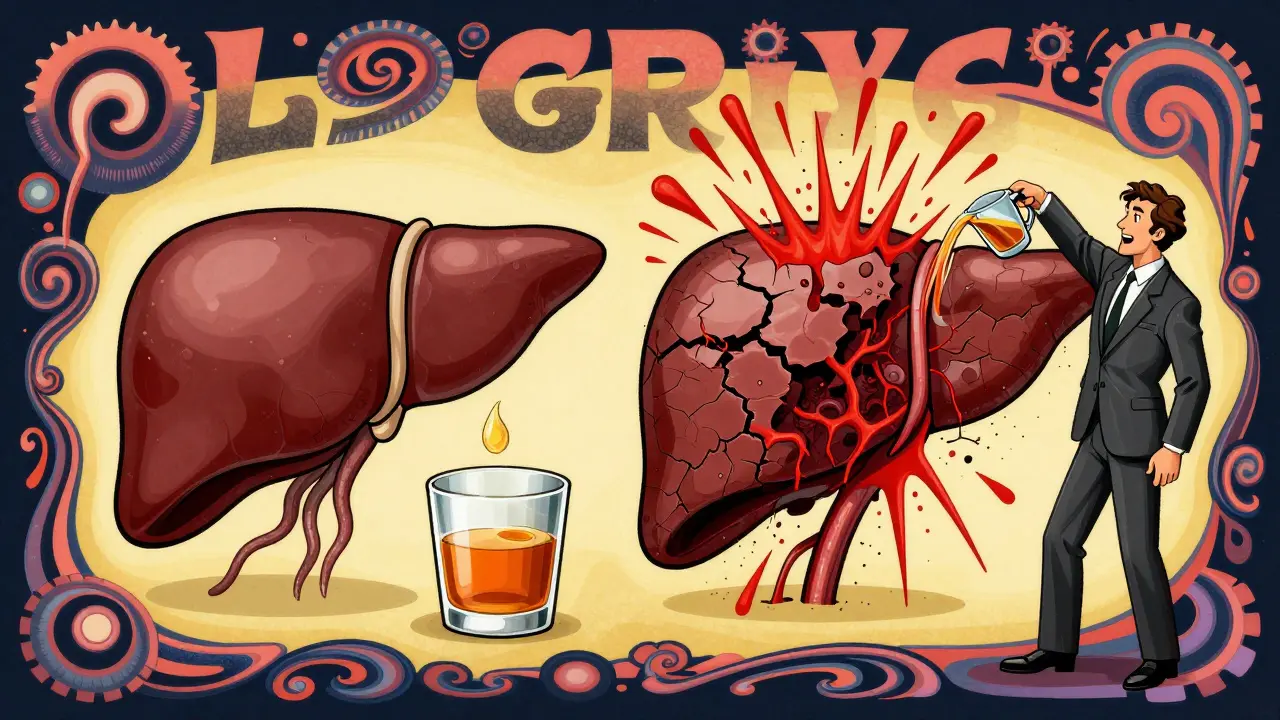
Alcoholic Liver Disease: Understanding the Stages from Fatty Liver to Cirrhosis

Most people don’t realize their drinking is slowly destroying their liver until it’s too late. By the time symptoms like yellow skin, swollen belly, or confusion show up, the damage is often advanced. Alcoholic liver disease doesn’t happen overnight. It creeps in quietly, stage by stage, and for many, it’s reversible-if they act early.
Stage 1: Fatty Liver (Hepatic Steatosis)
This is the first and most common stage. If you drink more than 4 units of alcohol a day-about 3 to 4 pints of beer or 3 small glasses of wine-you’re at risk. Around 90% of heavy drinkers develop fatty liver, sometimes in as little as 3 to 5 days. The liver gets overwhelmed and starts storing fat instead of processing it.
Here’s the good news: this stage has no symptoms in 95% of cases. No pain. No fatigue. No jaundice. You might feel fine. But blood tests can show elevated liver enzymes, especially AST and ALT, with AST usually higher than ALT. That’s a red flag.
What makes this stage different from the others? It’s fully reversible. Stop drinking for 4 to 6 weeks, and your liver can clear out the fat. One 2017 study found 85% of people who quit alcohol completely saw their fatty liver vanish. No medication needed. Just time and abstinence. The liver is an amazing organ-it regenerates. But only if you stop feeding it poison.
Stage 2: Alcoholic Hepatitis (Alcohol-Associated Hepatitis)
If you keep drinking after fatty liver, the next step is inflammation. This is alcoholic hepatitis, now called alcohol-associated hepatitis (AH) to reduce stigma. About 30-35% of people with fatty liver who keep drinking will develop this. It usually takes 5 to 10 years of heavy drinking, but sometimes it hits fast after a binge-like drinking 100 grams of alcohol (about 8 shots) in one day.
Symptoms start showing now. Jaundice (yellow eyes and skin) happens in 85% of moderate to severe cases. You might feel nauseous, lose your appetite, have fever, or feel achy. Your belly could swell from fluid buildup (ascites). In severe cases, you might get confused or drowsy-signs of hepatic encephalopathy, when toxins build up because the liver can’t filter them.
Doctors use the Maddrey Discriminant Function (mDF) score to measure severity. A score above 32 means you’re in danger. About 30-40% of people with severe AH die within a month if they don’t stop drinking and get treatment. Steroids like prednisolone can help, but only about 40% respond. The real treatment? Quitting alcohol. Immediately. If you stop, even severe cases can improve. If you don’t, you’re heading straight to cirrhosis.
Here’s something most don’t know: half the people with severe AH have never been told they have liver problems before. The disease hides until it’s loud.
Stage 3: Cirrhosis (Advanced Scarring)
Cirrhosis is when your liver turns to scar tissue. About 10-20% of long-term heavy drinkers reach this point. At this stage, more than 75% of healthy liver cells are replaced by fibrous scars. The organ can’t function properly. It’s no longer just inflamed-it’s broken.
People often think cirrhosis means the end. It doesn’t. But it’s not curable. The scarring is permanent. Still, stopping alcohol completely changes everything. In 50-60% of cases where cirrhosis is still compensated (meaning no major complications yet), abstinence can stop the damage and even improve survival. Without quitting, median survival drops to 1.8 years. With abstinence, it jumps to 12+ years.
Now the complications hit hard. Fluid builds up in the belly (ascites). Veins in the esophagus swell and can burst (variceal bleeding)-this kills 30% of cirrhotic patients over their lifetime. Kidney failure, brain fog, confusion, and even coma can follow. Liver cancer risk rises too-3-5% per year if you have cirrhosis.
Doctors use tools like FibroScan now instead of biopsies to check scarring. It’s faster, safer, and just as accurate. Treatments focus on managing symptoms: beta-blockers like propranolol cut bleeding risk by 45%. Lactulose helps with brain fog. But none of these fix the root cause.
The only cure left? A liver transplant. But most centers require 6 months of verified sobriety before even putting you on the list. That’s not punishment-it’s survival. Studies show 70-75% of transplant patients live at least 5 years after surgery.
Why Some People Progress Faster Than Others
Not everyone who drinks heavily gets cirrhosis. Why? Genetics, sex, and other health issues play a big role.
Women are more vulnerable. They develop liver damage after consuming less alcohol than men-sometimes half as much. That’s because their bodies process alcohol differently. Hormones and body fat make them absorb more alcohol into the bloodstream.
Genes matter too. If you carry certain variants like PNPLA3 or TM6SF2, your liver is more likely to scar. If you also have diabetes, high cholesterol, or obesity (metabolic syndrome), your risk doubles. Even moderate drinking speeds up liver damage if you already have fatty liver from sugar or carbs.
And then there’s viral hepatitis. If you have hepatitis B or C and drink, your liver gets hit from both sides. The damage multiplies.
One study found that people with fatty liver who drank 20-40 grams of alcohol daily (about 2 drinks) saw fibrosis progress 3 times faster than those who didn’t drink. Alcohol doesn’t just add damage-it accelerates everything.
Diagnosis: How Doctors Catch It Early
Most people aren’t diagnosed until they’re in the hospital with jaundice or bleeding. That’s too late. Early detection saves lives.
Doctors start with blood tests. Elevated AST and ALT, especially with AST more than twice ALT, is a classic sign. Gamma-GT and bilirubin levels also rise. But normal blood tests don’t mean a healthy liver. You can have advanced scarring and still have normal enzymes.
Ultrasound and FibroScan are now the go-to tools. FibroScan measures liver stiffness-harder liver = more scarring. It’s accurate 85-90% of the time for detecting moderate to severe fibrosis. No needles. No hospital stay. Just a quick scan.
Doctors also use scoring systems like the Glasgow Alcoholic Hepatitis Score (GAHS) or Lille Model to predict survival. A GAHS score above 9 means more than 50% chance of dying within 6 months without intervention.
The real challenge? Getting people tested before they’re sick. Only 1 in 3 heavy drinkers ever get screened. And many doctors don’t ask about alcohol use-because they’re afraid of offending patients.

What Works: Treatment and Recovery
There’s no magic pill. But there are proven paths to recovery.
Stage 1 (Fatty Liver): Quit drinking. That’s it. No drugs. No diet pills. Just stop. Most people see their liver enzymes return to normal in 6 weeks.
Stage 2 (Hepatitis): Stop drinking immediately. Add steroids if your mDF score is above 32. But steroids only help if you stop drinking. If you keep drinking, they won’t save you.
Stage 3 (Cirrhosis): Abstinence is non-negotiable. Manage complications with medication. Avoid NSAIDs like ibuprofen-they hurt the liver. Get vaccinated for hepatitis A and B. Screen for liver cancer every 6 months with ultrasound and AFP blood tests.
Emerging treatments show promise. Fecal microbiota transplants (FMT) from healthy donors improved survival in 40% of severe AH patients in a 2022 study. New drugs like emricasan are being tested to reduce inflammation without steroids.
But the most powerful treatment? Support. People who get help from addiction specialists alongside liver doctors are twice as likely to stay sober. One 2023 study showed 65% abstinence at 1 year with combined care-compared to 35% with liver care alone.
What Doesn’t Work: Denial and Delay
Many patients say, “I only drink on weekends.” Or, “I’m not an alcoholic.” But alcohol-associated liver disease doesn’t care about labels. It cares about total dose over time.
One Reddit user wrote: “My doctor told me I had fatty liver at 38. I thought, ‘I’ll cut back.’ I didn’t quit. Three years later, I was in the hospital with cirrhosis.”
Another said: “I had three hospitalizations for alcoholic hepatitis. Each time, I swore I’d stop. Each time, I started again. By year four, I was told I needed a transplant-but I wasn’t eligible because I hadn’t quit long enough.”
Stigma kills. Many patients report being judged by doctors, family, even friends. That shame makes them hide their drinking. And silence kills faster than alcohol.
Here’s the truth: you don’t have to be an ‘alcoholic’ to have ALD. You just have to drink too much, too often. And you don’t have to hit rock bottom to save your liver. You just have to stop.
What You Can Do Today
Don’t wait for symptoms. If you drink regularly, get checked.
- Ask your doctor for a FibroScan or liver ultrasound.
- Request blood tests: AST, ALT, GGT, bilirubin.
- If you drink more than 14 units a week (UK guideline), consider cutting back or quitting.
- If you’ve been diagnosed with fatty liver, treat it like a warning siren-not a suggestion.
- Reach out for support. Groups like Alcoholics Anonymous, or even online forums, can help you stay sober.
Your liver doesn’t scream. It whispers. And if you ignore the whisper, it eventually stops talking altogether.
Can you reverse alcoholic liver disease?
Yes-but only if you stop drinking and act early. Fatty liver reverses in 4-6 weeks with complete abstinence. Alcoholic hepatitis can improve if caught early and treated with steroids and sobriety. Cirrhosis can’t be undone, but stopping alcohol can stabilize it and extend life by decades.
How much alcohol causes liver damage?
As little as 3-4 units a day (about 2-3 pints of beer or 2 small glasses of wine) can cause fatty liver in as little as a week. Heavy drinking-more than 60-80 grams daily (5-6 drinks)-over 5-10 years raises the risk of cirrhosis. Women are at higher risk at lower doses due to differences in metabolism.
Does quitting alcohol help if you already have cirrhosis?
Absolutely. Even with cirrhosis, stopping alcohol improves survival dramatically. People who quit have a 70-90% chance of surviving 5 years if their cirrhosis is still compensated. Those who keep drinking survive less than 2 years on average. Abstinence is the most effective treatment at any stage.
Can you drink moderately after recovering from fatty liver?
No. Once your liver has been damaged by alcohol, even small amounts can restart the damage. Studies show that returning to moderate drinking after fatty liver leads to faster progression to hepatitis and cirrhosis. Complete abstinence is the only safe choice.
Are there any medications to cure alcoholic liver disease?
No cure exists, but treatments help manage stages. Steroids like prednisolone are used for severe alcoholic hepatitis. Beta-blockers prevent bleeding in cirrhosis. Lactulose helps with brain fog. New drugs and microbiome therapies are in trials, but none replace the need to stop drinking.
Ashley Porter
January 24, 2026 AT 20:35AST > ALT is such a classic red flag it’s almost poetic. I’ve seen it in ERs - patients walking in like nothing’s wrong, labs screaming otherwise. Liver’s a silent assassin until it’s not.
Also, FibroScan is a game-changer. No more invasive biopsies for screening. Why aren’t primary docs pushing this harder?