Allergy Medications: Antihistamines and Decongestants Risks You Can't Ignore
Every year, millions of people reach for antihistamines and decongestants to chase away sneezing, stuffy noses, and itchy eyes. These medications are everywhere - on supermarket shelves, in pharmacy aisles, even in convenience stores. They’re cheap, easy to grab, and feel like a quick fix. But here’s the truth most people don’t talk about: antihistamines and decongestants aren’t harmless. They carry real, sometimes dangerous, risks - especially if you’re over 65, have high blood pressure, or are taking other meds.
How These Meds Work (And Why That Matters)
Antihistamines block histamine, the chemical your body releases during an allergic reaction. That stops sneezing, runny nose, and itching. But not all antihistamines are the same. First-generation ones like diphenhydramine (Benadryl) and doxylamine (Unisom) cross into your brain. That’s why they make you drowsy - sometimes so badly you can’t drive or operate machinery. Second-generation ones like loratadine (Claritin) and cetirizine (Zyrtec) don’t cross the blood-brain barrier as easily, so they’re less likely to knock you out. But they’re not risk-free. Decongestants like pseudoephedrine (Sudafed) and phenylephrine shrink swollen blood vessels in your nose. That’s how they clear congestion fast. But they don’t just shrink blood vessels in your nose. They shrink them everywhere - including in your heart and brain. That’s why your heart might race, your blood pressure spikes, or you feel jittery and anxious.The Hidden Dangers of First-Generation Antihistamines
If you’re over 65, you need to hear this: diphenhydramine and doxylamine are on the Beers Criteria list of medications older adults should avoid. Why? Because they’re anticholinergic. That means they block a brain chemical called acetylcholine, which controls memory, muscle movement, and bladder function. In older adults, this leads to:- Confusion and memory problems - up to 50% more likely
- Blurred vision and dry mouth
- Constipation and trouble urinating
- A 300% higher risk of falling
Decongestants: The Silent Blood Pressure Threat
Pseudoephedrine and phenylephrine are sold as if they’re safe for everyone. But they’re not. If you have high blood pressure - and nearly 116 million American adults do - these meds can push your numbers into dangerous territory. Mayo Clinic data shows decongestants can raise systolic blood pressure by 5-10 mmHg. That might sound small. But for someone with uncontrolled hypertension, that spike can trigger a heart attack or stroke. And it doesn’t take much. One pill, taken with coffee or an energy drink, can be enough. Nasal sprays like oxymetazoline (Afrin) seem safer because they’re local. But they’re not. Using them for more than three days? You’ve got a 50% chance of rebound congestion - your nose gets worse after you stop. Now you’re stuck in a cycle: spray to feel better, stop and feel worse, spray again. It’s called rhinitis medicamentosa. And it’s hard to break.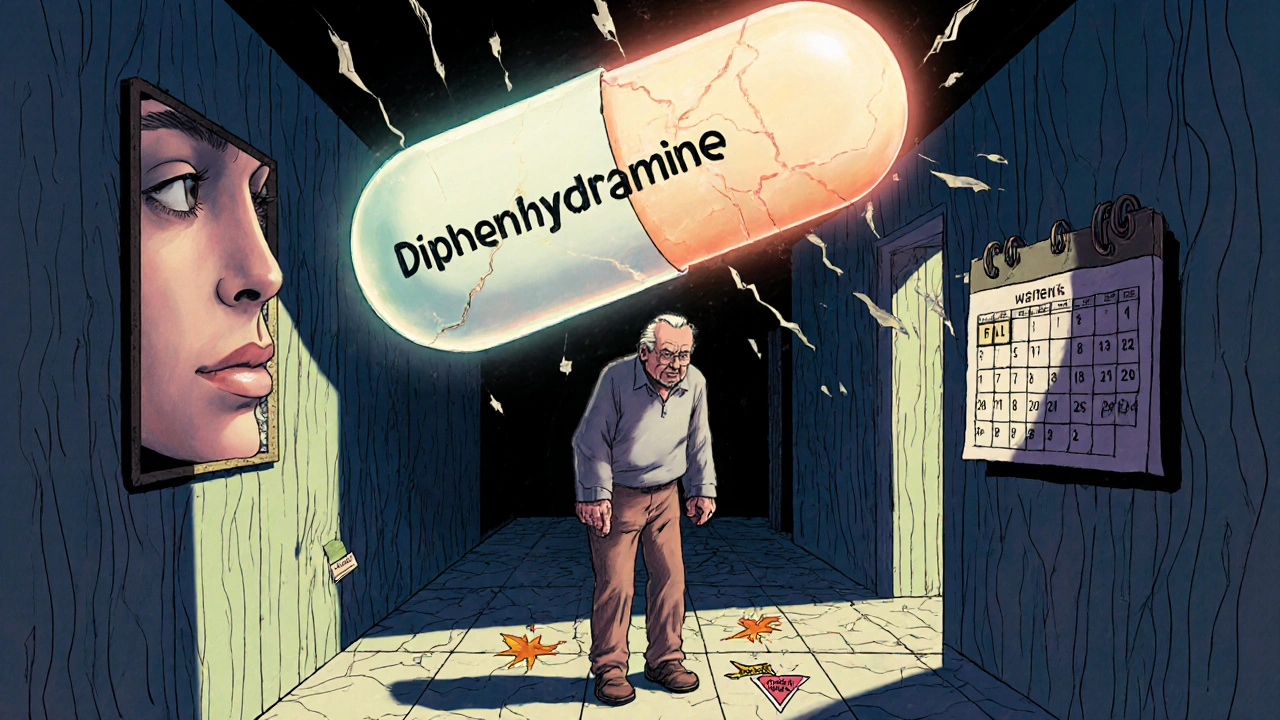
Combination Products Are a Minefield
You see them everywhere: “All-in-One Cold & Allergy Relief.” “Nighttime Sinus & Flu.” “Maximum Strength Congestion & Cough.” These products mix antihistamines, decongestants, painkillers, and cough suppressants. And that’s the problem. You might not realize you’re taking two doses of acetaminophen (Tylenol) - one in the cold med, one in the painkiller you took earlier. The daily limit is 4,000 mg. Go over that, and you risk liver failure. You don’t need to overdose dramatically. Just taking an extra tablet a day for three days can do it. And then there’s the antihistamine added to the mix. If you have an enlarged prostate - common in men over 50 - that antihistamine can make it impossible to pee. You end up in the ER with a full bladder.Who Should Never Take These Meds?
The NHS and FDA list clear red flags. Don’t take decongestants if you have:- High blood pressure
- Heart disease
- Diabetes
- Thyroid problems
- Enlarged prostate
- Glaucoma
- Liver or kidney disease
- Seizure disorders
- Bladder problems
- Severe dry mouth or constipation
Medication Interactions That Can Kill
People don’t think about drug interactions with OTC meds. But they should. Taking a decongestant with an SSRI antidepressant (like sertraline or fluoxetine)? You’re risking a hypertensive crisis - blood pressure can shoot over 180 mmHg. That’s a medical emergency. Mixing antihistamines with alcohol? You’re doubling the sedation. That’s why older adults on Benadryl and a glass of wine are four times more likely to fall. And don’t forget MAOIs - older antidepressants like phenelzine. Taking a decongestant within two weeks of stopping one of these can cause a deadly spike in blood pressure. That’s why the Mayo Clinic says: never mix them. Even energy drinks are a problem. Caffeine + pseudoephedrine = racing heart, panic attacks, chest pain. Rutgers University’s poison control center saw a 25% jump in calls from young adults mixing OTC allergy meds with energy drinks in 2022.
What to Do Instead
If your allergies last more than 10-14 days, it’s not allergies anymore. It’s probably a sinus infection - and antihistamines can make it worse by thickening mucus. Mayo Clinic says 25% of patients with sinus infections get worse on antihistamines. Here’s what actually works:- Saline nasal rinses - safe, cheap, and effective
- Intranasal corticosteroids (like fluticasone) - better than decongestants for chronic congestion
- Allergy shots or tablets - for long-term relief
- Humidifiers and air filters - reduce triggers at home
When to See a Doctor
You don’t need to suffer. But you also don’t need to guess. See your doctor if:- Your symptoms last more than two weeks
- You’re using OTC meds more than twice a week
- You have high blood pressure, heart disease, or are over 65
- You’re taking any prescription meds
- You’ve had side effects like rapid heartbeat, confusion, or trouble urinating
The Bottom Line
OTC doesn’t mean risk-free. Antihistamines and decongestants are powerful drugs. They can help - but they can also hurt. If you’re over 65, have heart issues, or take other meds, you’re at higher risk. And if you’re using them long-term, you’re probably making things worse. Stop treating symptoms like they’re just annoying. Start treating them like they’re signals. Your body is telling you something. Maybe it’s allergies. Maybe it’s something else. Either way, don’t reach for the bottle without asking: Is this really safe for me?Can I take antihistamines every day for allergies?
Second-generation antihistamines like loratadine or cetirizine are generally safe for daily use in healthy adults. But first-generation ones like diphenhydramine should never be used daily - they cause drowsiness, memory issues, and increase fall risk. If you need daily meds, talk to your doctor. You might need a nasal spray or allergy testing instead.
Are decongestants safe if I have high blood pressure?
No. Decongestants like pseudoephedrine and phenylephrine can raise your blood pressure by 5-10 mmHg, which may trigger a heart attack or stroke in someone with uncontrolled hypertension. Even if your BP is “normal,” these meds can push it into danger. Use saline rinses or intranasal corticosteroids instead.
Why do some allergy meds make me feel wired or anxious?
That’s likely the decongestant. Pseudoephedrine stimulates your nervous system, causing jitteriness, rapid heartbeat, and anxiety. It’s not just “being sensitive.” It’s a direct effect. If you feel this way, switch to a product without a decongestant - or try a second-generation antihistamine alone.
Can antihistamines cause weight gain?
Some people report weight gain with long-term antihistamine use, especially first-generation ones. The reason isn’t fully understood, but it may be linked to increased appetite or slowed metabolism due to drowsiness. If you’re gaining weight while on daily antihistamines, talk to your doctor - there may be better options.
Is it safe to give my child an OTC allergy med?
No. The FDA warns that OTC cough and cold medicines containing antihistamines or decongestants should never be given to children under 2. Between 1969 and 2006, over 120 children died from these products. Even older kids can have dangerous reactions like seizures or rapid heart rates. Always check with a pediatrician first.
What’s the safest way to treat seasonal allergies?
The safest long-term approach is avoiding triggers and using intranasal corticosteroids like fluticasone. These reduce inflammation without the side effects of antihistamines or decongestants. For quick relief, second-generation antihistamines are safer than first-gen. Saline rinses and HEPA filters at home also help. If symptoms persist, see an allergist - you may benefit from immunotherapy.
fiona collins
November 24, 2025 AT 21:48Just stopped taking Benadryl last week-woke up with itching so bad I thought I had scabies. No rash. No bites. Just… burning. Took three days to fade. No one warned me.
giselle kate
November 26, 2025 AT 11:39Of course the government lets these dangerous pills sit next to candy. America’s gone soft. If you can’t read a label, you deserve what you get. Stop blaming the meds and start blaming the lazy.
Karen Willie
November 28, 2025 AT 11:38I used to rely on Sudafed every winter until my BP spiked. Now I use a neti pot and a humidifier. It’s not as fast, but I sleep better. And I’m still here. 💕
Leisha Haynes
November 30, 2025 AT 09:50So you're telling me the same stuff my grandma took in the 70s is still killing people? Wow. What a surprise. At least they had the decency to warn us on the box back then. Now? It's all glitter and hashtags. 🙄
Shivam Goel
December 1, 2025 AT 00:12Let’s analyze the data: First-gen antihistamines have a half-life of 4-8 hours, but anticholinergic burden accumulates over time. Studies show a 1.5x increased dementia risk after 90 days of daily use. The Beers Criteria isn’t a suggestion-it’s a red alert. And the 300% fall risk? That’s not anecdotal-it’s meta-analyzed. If you’re over 65, you’re not ‘just tired’-you’re pharmacologically impaired.
Andrew McAfee
December 2, 2025 AT 08:04Back home in Lagos, we use ginger tea and steam inhalation. No pills. No side effects. Why are we so quick to swallow chemicals when nature gave us solutions? It's not just about health-it's about cultural disconnect.
Roscoe Howard
December 2, 2025 AT 19:17It is, indeed, a matter of profound concern that the pharmaceutical-industrial complex has normalized the casual consumption of pharmacologically potent agents under the misleading rubric of 'over-the-counter.' The absence of medical oversight in the procurement of these substances constitutes a systemic failure of public health governance.
Kimberley Chronicle
December 3, 2025 AT 16:48From a clinical perspective, the anticholinergic burden metric is underutilized in primary care. We need better screening tools-like the Anticholinergic Cognitive Burden Scale-to flag high-risk polypharmacy before it leads to ER visits. Also, saline irrigation has a Level 1A evidence base for chronic rhinosinusitis. Why isn’t this first-line?
Shirou Spade
December 4, 2025 AT 07:30Medicine is not a weapon against nature-it’s a conversation. When we silence symptoms with chemicals, we ignore the message. Allergies aren’t enemies. They’re signals. Maybe your body is asking for cleaner air. Or less sugar. Or less stress. The pill is the easy answer. But the real work? That’s harder.
Lisa Odence
December 4, 2025 AT 14:12Okay but like... did you know that some antihistamines can literally make you gain weight?? 😱 I gained 12 lbs on Zyrtec and no one told me! My doctor was like 'oh that's rare' but then I read 17 studies and it's not rare at all. Also, don't mix with caffeine. I had a panic attack after a coffee and Sudafed. My heart was doing the cha-cha. 🫠
Patricia McElhinney
December 4, 2025 AT 16:48Anyone who takes Benadryl daily is either ignorant or reckless. The FDA has issued MULTIPLE warnings. The Beers Criteria exists for a reason. And if you're giving OTC meds to your kids? You're not a parent-you're a liability. This isn't opinion. It's fact. And if you don't believe me, go read the prescribing info. It's not hard.
Dolapo Eniola
December 5, 2025 AT 17:11Y’all in the US think pills fix everything. In Nigeria, we know the body heals itself. We use neem leaves, turmeric, and prayer. No drugs. No side effects. You think you’re smart with your science? Nah. You’re just addicted to chemicals. 🙏🔥