Aspirin Therapy for Heart Disease Prevention: Who Should Take It in 2025?
For decades, taking a daily low-dose aspirin was something millions of people did without thinking - like brushing their teeth. It was the go-to move for preventing heart attacks, especially if you had a family history or were over 50. But here’s the truth: aspirin therapy for heart disease prevention isn’t what it used to be. In 2025, the advice has flipped. For most healthy adults, taking aspirin daily to prevent a first heart attack or stroke is no longer recommended - and in some cases, it could be dangerous.
Why Aspirin Was Once a No-Brainer
Aspirin works by thinning the blood. It blocks a chemical in platelets that makes them stick together and form clots. If a clot blocks an artery in your heart or brain, it can cause a heart attack or stroke. For people who already had one, aspirin cuts the chance of another by about 21%. That’s why it’s still a cornerstone of secondary prevention - meaning after you’ve had a heart event.
But for people without any history of heart disease? The math changed. Back in the 1980s and 90s, studies like the Physicians’ Health Study showed aspirin reduced heart attacks in men. That led to widespread adoption. But those studies were done before statins, before blood pressure meds were as good, before we understood how much smoking, diet, and exercise matter. Today, people manage their risk better. And the bleeding risk from aspirin? It’s real - and growing.
Who Should Still Consider Aspirin? (The Narrow Group)
The 2022 US Preventive Services Task Force (USPSTF) guidelines are clear: don’t start aspirin if you’re 60 or older. Period. For adults between 40 and 59, it’s not a blanket yes. It’s a maybe - and only if you meet very specific conditions.
You might consider aspirin if:
- You’re between 40 and 59 years old
- Your 10-year risk of heart disease is 10% or higher
- You have no increased risk of bleeding
- You’re willing to take it for at least 10 years
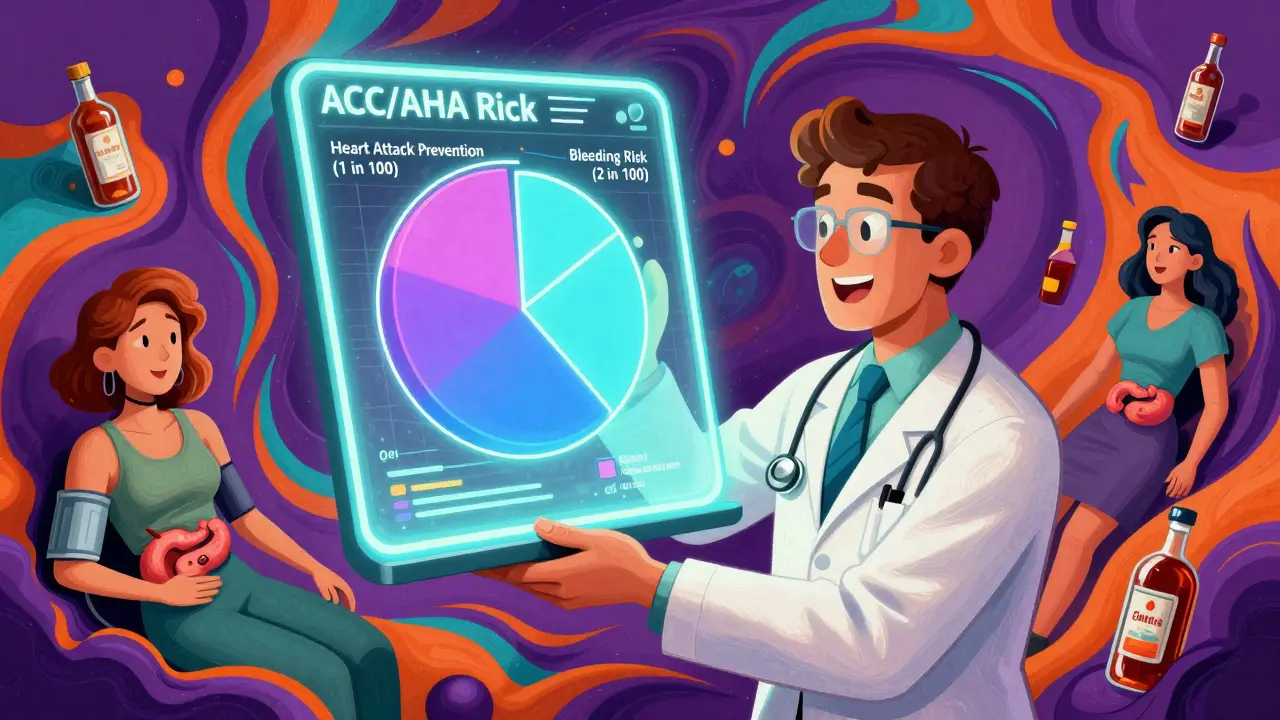
How do you know your 10-year risk? Doctors use a tool called the ACC/AHA pooled cohort equation. It asks for your age, sex, race, blood pressure, cholesterol levels, whether you have diabetes, and if you smoke. You can’t guess this. You need your latest lab results and a doctor’s input.
For example: a 55-year-old man with high LDL cholesterol, untreated high blood pressure, and who smokes might hit that 10% threshold. A 52-year-old woman with normal numbers and no smoking history? Probably not. That’s why blanket advice doesn’t work.
Who Should Avoid Aspirin Completely?
Aspirin isn’t harmless. It’s a drug with serious side effects - especially for older adults.
Stop or never start aspirin if you have:
- A history of stomach ulcers or GI bleeding
- Active liver or kidney disease
- Use of blood thinners like warfarin or apixaban
- Uncontrolled high blood pressure
- Age 60 or older (even if you think you’re healthy)
- Drink alcohol regularly (more than 2-3 drinks a day)
The HAS-BLED score is a simple checklist doctors use to spot bleeding risk. If you score 3 or higher, aspirin is a bad idea. Even one of these factors - like being over 65 or on NSAIDs like ibuprofen - can tip the scales.
Here’s what the numbers show: for every 100 people like you taking aspirin daily for 10 years, about 1 might avoid a heart attack. But 2 might have a major bleeding event - like a stomach bleed or brain hemorrhage - that requires hospitalization or a blood transfusion. That’s not a trade-off most people want to make.

What About Diabetes or Family History?
Many people think: “My dad had a heart attack at 58. I should take aspirin.” Or “I have type 2 diabetes - doesn’t that mean I need it?”
The answer? Maybe - but not automatically.
The American Diabetes Association says aspirin can be considered for people with diabetes over 40 who have additional risk factors - like high blood pressure, smoking, or kidney disease. But even then, it’s not a default. A 2020 study in Atherosclerosis found that in people with diabetes and low coronary calcium scores, aspirin offered no benefit. In those with high scores? Possibly. But you need a scan to know.
Family history alone? Not enough. Genetics matter, but they don’t override bleeding risk. A 62-year-old with a strong family history but normal cholesterol, no smoking, and no high blood pressure has a low overall risk. For them, aspirin does more harm than good.
What Are the Real Alternatives?
If aspirin isn’t the answer for primary prevention, what is?
Statins. That’s it. For most people, the best way to prevent a first heart attack is to lower cholesterol with a statin like atorvastatin or rosuvastatin. They reduce heart attack risk by 25-37% - far more than aspirin’s 10-15%. And they don’t cause bleeding.
Other proven tools:
- Keeping blood pressure under 130/80
- Walking 150 minutes a week
- Stopping smoking
- Eating more vegetables, nuts, whole grains
- Losing excess weight
These aren’t just “lifestyle tips.” They’re medical interventions with stronger evidence than aspirin for people without heart disease. And they come with zero bleeding risk.
Why Are So Many People Still Taking It?
Despite the guidelines, an estimated 22 million Americans still take daily aspirin for primary prevention. Why?
Old habits die hard. Many people were told to take it by a doctor 15 years ago - and never got an update. Others rely on anecdotal stories: “My neighbor took it for 30 years and never had a heart attack.” Or “My cardiologist said keep going because of my family history.”
But doctors aren’t always up to date. A 2021 study found only 43% of primary care physicians could correctly calculate a patient’s 10-year heart risk. Many still default to prescribing aspirin because it’s cheap, familiar, and patients expect it.
On Reddit and health forums, you’ll see people debating whether to stop. One user wrote: “I stopped aspirin at 67 after my doctor said I shouldn’t take it. I had three nosebleeds in six months - I thought it was the aspirin. Turns out it was dry winter air. But I was terrified.” Another said: “I had a heart attack at 68. I’ve taken aspirin since 55. My doctor says I owe it to the aspirin.”
These stories sound convincing. But they’re not data. They’re survivorship bias - you only hear from the people who made it. You don’t hear from the ones who bled out.
What If You’re Already Taking Aspirin?
If you’re currently taking daily aspirin and you’re over 60 - or you have any bleeding risk - talk to your doctor. Don’t stop cold turkey. Abruptly stopping aspirin can, in rare cases, trigger a rebound clotting effect. But if you’re over 60 with no heart disease, the odds are you’re better off without it.
If you’re under 60 and have no risk factors? You probably don’t need it. If you’re under 60 and have high risk? Ask your doctor to run your 10-year score. If it’s below 10%, skip it. If it’s above 10%, discuss the pros and cons - not just with your doctor, but with yourself.
Ask yourself: Do I understand the bleeding risk? Am I okay with a 1 in 50 chance of a serious bleed over 10 years to get a 1 in 100 chance of avoiding a heart attack? If you’re not sure, don’t take it.
Bottom Line: Aspirin Isn’t a Vitamin
Aspirin is not a supplement. It’s a drug. It has risks. It has benefits. And for most healthy people in 2025, the risks outweigh the benefits.
The era of “take a baby aspirin every day” is over. What’s replacing it? Better risk assessment. Better cholesterol control. Better lifestyle habits. And a shift away from one-size-fits-all medicine.
If you’re unsure, don’t guess. Get your 10-year risk calculated. Get your bleeding risk checked. Talk to your doctor - not about what you’ve heard on the internet, but about your actual numbers. Your heart might thank you. So might your stomach.
Should I take aspirin daily to prevent a heart attack if I’m over 60?
No. Major guidelines from the US Preventive Services Task Force and the American Heart Association recommend against starting aspirin for heart disease prevention in adults 60 or older. The risk of serious bleeding - including stomach or brain bleeds - is higher than the chance of preventing a first heart attack or stroke in this age group. Even if you feel healthy, the net harm outweighs any benefit.
What if I have diabetes? Do I still need to avoid aspirin?
Not necessarily. For people with diabetes over 40 who also have other risk factors - like high blood pressure, smoking, or kidney disease - aspirin may still be considered. But it’s not automatic. Your doctor should calculate your 10-year heart disease risk and check your bleeding risk before recommending it. If your risk is low, aspirin won’t help. If your risk is high, the benefit might be worth it - but only after a full discussion.
Is 81 mg aspirin safer than 325 mg for prevention?
Yes. For prevention, only low-dose aspirin - 75 to 100 mg daily - is recommended. That’s usually the 81 mg tablet sold as “baby aspirin.” Higher doses (like 325 mg) don’t offer more protection but significantly increase bleeding risk. Never take regular-strength aspirin daily unless prescribed for another reason, like after a stent or heart attack.
Can I take aspirin if I’m already on a statin?
Yes - but only if you’re in the small group that still benefits from aspirin. Statins are the main tool for preventing first heart attacks. Aspirin adds little extra benefit if you’re already on a statin and have your blood pressure and cholesterol under control. For most people, adding aspirin just adds bleeding risk without meaningful gain. Your doctor should weigh both drugs together, not assume aspirin is automatically helpful.
What are the signs I might be bleeding from aspirin?
Watch for: black or tarry stools, vomiting blood (looks like coffee grounds), unexplained bruising, nosebleeds that won’t stop, headaches with dizziness (could signal brain bleed), or unusually pale skin and fatigue (signs of anemia from slow bleeding). If you notice any of these, stop aspirin and call your doctor immediately. Don’t wait.
How do I know my 10-year heart disease risk?
Your doctor uses a calculator called the ACC/AHA Pooled Cohort Equation. It needs your age, sex, race, total cholesterol, HDL, systolic blood pressure, whether you have diabetes, and if you smoke. Most electronic health records calculate this automatically during a check-up. If yours doesn’t, ask for it. You can’t guess your risk - you need the numbers.
Should I stop aspirin if I’ve been taking it for years?
Don’t stop suddenly without talking to your doctor. If you’re over 60 and have no history of heart disease, the chances are you should stop. But your doctor may want you to taper off slowly, especially if you’ve been on it for a long time. Never stop because you read something online - get professional advice based on your personal health record.
Are there any groups who should still take aspirin for prevention?
Yes - but they’re rare. People with familial hypercholesterolemia (a genetic condition causing very high cholesterol from birth) may still benefit. Also, some people with very high coronary artery calcium scores (over 300) might be candidates. These are exceptions, not the rule. They require detailed testing and a specialist’s input - not a general recommendation.
Michelle M
December 15, 2025 AT 12:25It’s wild how we’ve gone from treating aspirin like a vitamin to recognizing it as a real drug with real trade-offs. I used to take it daily because my dad did - until I read the bleeding risk stats and realized I was gambling with my stomach for a 1% benefit. Sometimes the most powerful health decision is knowing when *not* to do something.
Melissa Taylor
December 15, 2025 AT 16:34This is exactly the kind of nuanced, science-backed update we need more of. So many people are still on aspirin out of habit, not knowledge. Kudos to the author for breaking it down without fear or fluff. It’s not about fearmongering - it’s about informed choice.
Cassie Henriques
December 17, 2025 AT 15:13ACC/AHA pooled cohort equation is non-negotiable here. If your doc hasn’t run your 10-year ASCVD risk, they’re practicing 2005 medicine. And let’s be real - statins are the real MVPs for primary prevention. Aspirin’s role is now just a footnote in high-risk subgroups. No more blanket prescriptions. Period.
Lisa Davies
December 18, 2025 AT 03:14My grandma took aspirin every day for 40 years. She’s 92, hikes every morning, and still makes the best apple pie. But she also had a GI bleed at 78 and needed a transfusion. She didn’t know why. Now I tell everyone: don’t assume it’s harmless. Talk to your doc. 🙏
Mike Nordby
December 19, 2025 AT 01:32The shift in guidelines reflects a broader evolution in preventive medicine: from one-size-fits-all interventions to risk-stratified, evidence-based decisions. Aspirin’s decline as a primary prevention tool is not a failure of medicine - it’s a sign of progress. We now understand that the absence of harm is not the same as the presence of benefit.
RONALD Randolph
December 20, 2025 AT 10:48Who let the bureaucrats decide this?! I’ve taken 81mg since I was 50 - no bleeding, no problems. Now you want me to stop because some study says ‘maybe’? I’ll take my chances. My heart’s still beating - and so is my stomach. Stop over-medicalizing everything!
John Brown
December 22, 2025 AT 08:51My doctor finally ran my risk score last year - turned out I was at 8.7%. She said aspirin wasn’t worth it. I was shocked. I thought I was doing the right thing. Now I’m on a statin, walking 5 days a week, and eating way more veggies. Feels better than popping a pill I didn’t need.
Sai Nguyen
December 22, 2025 AT 11:19Western medicine is broken. In India, we know aspirin saves lives. You Americans overthink everything. One pill, one life. Why complicate? Your doctors are scared of lawsuits, not patients.
Benjamin Glover
December 24, 2025 AT 10:27How quaint. The American healthcare system still clings to outdated paradigms while the rest of the world has moved on to precision prevention. The fact that 22 million are still on aspirin is less a testament to public health literacy and more a reflection of systemic inertia.
Nupur Vimal
December 24, 2025 AT 19:58Everyone’s so scared of bleeding they forget aspirin stops heart attacks. My uncle had one at 61 and he’s alive because he took it. You can’t just throw out a tool because some numbers say so. You need to think with your heart not your spreadsheet
Raj Kumar
December 25, 2025 AT 09:52my doc said i need to get my calcium score done before even thinking about aspirin. turns out mine was 120 - low risk. so i stopped. now i just walk, eat nuts, and chill. no more pills for no reason. feels good to be proactive without being reckless
John Samuel
December 26, 2025 AT 02:39Aspirin, once the unsung hero of the medicine cabinet, now stands as a relic of medical paternalism - a blunt instrument in an age of scalpel-like precision. We have moved beyond the era of prophylactic pharmacology for the asymptomatic; we now inhabit a realm where individualized risk calculus, lipid profiling, and arterial imaging dictate therapeutic pathways. To persist in aspirin’s indiscriminate use is to confuse the virtue of precaution with the vice of complacency.
Jake Sinatra
December 26, 2025 AT 16:13Just stopped my aspirin after reading this. I’m 58, no heart issues, but had a minor nosebleed last month. Didn’t connect it until now. My doctor ran the numbers - 7.3% risk. Not worth it. I’m switching focus to my blood pressure and walking. Thanks for the clarity - this is the kind of info we need, not fear or hype.