Compare Hypernil (Lisinopril) with Alternatives: What Works Best for High Blood Pressure?

If you're taking Hypernil for high blood pressure, you're not alone. Millions of people in the UK and worldwide rely on lisinopril to keep their numbers in check. But what if it’s not working well for you? Or maybe you’re dealing with a dry cough, dizziness, or just wondering if there’s something better out there? You’re not overreacting-switching medications is a common and smart move when your current one isn’t quite right.
What Exactly Is Hypernil?
Hypernil is just a brand name for lisinopril, a generic ACE inhibitor used to treat high blood pressure (hypertension), heart failure, and sometimes kidney problems in diabetics. It works by relaxing blood vessels so your heart doesn’t have to pump as hard. That lowers your blood pressure and reduces strain on your heart and kidneys.
Lisinopril is taken once a day, usually in the morning. It’s cheap, widely available on the NHS, and has been used since the 1980s. But while it’s effective for many, it’s not perfect for everyone. Side effects like persistent dry cough (affecting up to 20% of users), swelling in the face or throat (rare but serious), and low blood pressure are common reasons people look for alternatives.
Why Consider Alternatives to Hypernil?
There are three main reasons people switch away from lisinopril:
- Side effects-especially that annoying dry cough that won’t go away
- Not lowering blood pressure enough-some people need a stronger or different type of drug
- Other health conditions-like kidney disease, diabetes, or pregnancy
Studies show that about 1 in 5 people stop taking ACE inhibitors like lisinopril because of side effects. That’s a lot. And if you’re one of them, you’re not failing-you just need a different tool.
Top Alternatives to Hypernil (Lisinopril)
There are several well-researched, NHS-approved alternatives. Each works differently, so what’s best depends on your body and your health history.
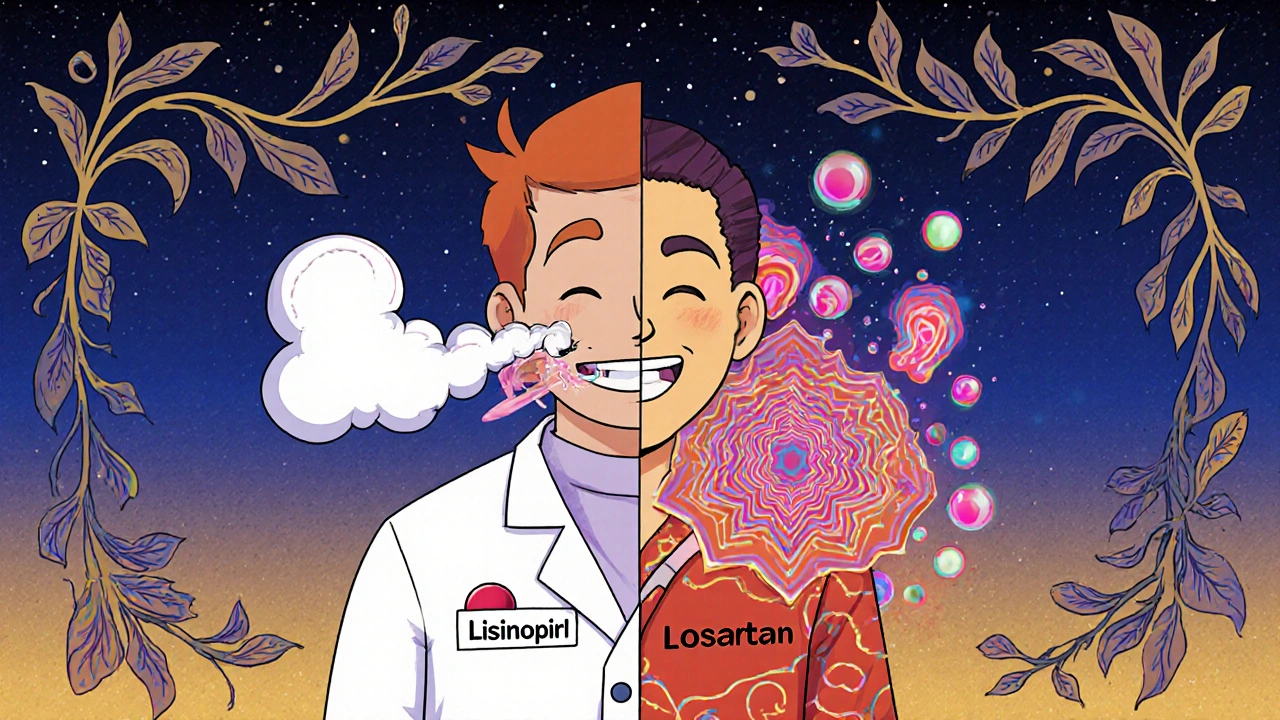
1. Losartan (Cozaar)
Losartan is an ARB-angiotensin II receptor blocker. It does almost the same job as lisinopril but blocks a different step in the blood pressure pathway. The big win? It rarely causes a dry cough. In fact, studies comparing losartan and lisinopril found cough rates dropped from 20% to under 5%.
Losartan is often the first choice when someone can’t tolerate lisinopril. It’s also been shown to protect kidneys in people with type 2 diabetes better than some other drugs. It’s available as a generic, costs about the same as lisinopril, and is taken once daily.
2. Amlodipine (Norvasc)
Amlodipine is a calcium channel blocker. Instead of relaxing blood vessels by blocking hormones, it blocks calcium from entering muscle cells in your arteries. This makes them widen naturally.
It’s especially good for older adults and people of African or Caribbean descent, who often respond better to calcium channel blockers than ACE inhibitors. It doesn’t cause coughing. The downside? Some people get swollen ankles or feel flushed. But for many, it’s a better fit.
The ALLHAT trial (one of the largest blood pressure studies ever) showed amlodipine was just as effective as lisinopril at preventing heart attacks and strokes-and had fewer side effects overall in certain groups.
3. Hydrochlorothiazide (HCTZ)
Hydrochlorothiazide is a thiazide diuretic. It’s a water pill-helps your kidneys get rid of extra salt and water. This reduces blood volume, which lowers pressure in your vessels.
It’s often used in combination with other drugs, but many people start with it alone, especially if they’re older or have mild hypertension. It’s cheap, effective, and has been around since the 1950s. Side effects can include low potassium, dizziness, or increased urination.
Research from the British Hypertension Society shows that for many patients, especially over 55, HCTZ is just as good as lisinopril-and sometimes better at preventing strokes.
4. Valsartan (Diovan)
Valsartan is another ARB, similar to losartan. It’s slightly stronger in lowering blood pressure and may be preferred if you have heart failure after a heart attack.
It’s taken once a day. Side effects are mild-dizziness, fatigue, or stomach upset. Like losartan, it avoids the cough issue. It’s a bit more expensive than losartan but still widely available on the NHS.
5. Ramipril (Altace)
Ramipril is another ACE inhibitor, like lisinopril. So why consider it? Because not all ACE inhibitors are the same.
Some people tolerate ramipril better than lisinopril. It’s often used in people with heart failure or after a heart attack because it’s been shown to reduce death rates in those groups. But if you had a cough with lisinopril, you’re likely to get it with ramipril too-so it’s not a good swap if cough is your main issue.
Comparison Table: Hypernil vs. Top Alternatives
| Medication | Class | Common Side Effects | Best For | Cough Risk | Cost (NHS) |
|---|---|---|---|---|---|
| Hypernil (Lisinopril) | ACE inhibitor | Dry cough, dizziness, fatigue, high potassium | General hypertension, heart failure, diabetic kidney protection | High (up to 20%) | £2-£5/month |
| Losartan | ARB | Dizziness, fatigue, high potassium | People with ACE inhibitor cough, diabetes, kidney disease | Low (under 5%) | £2-£6/month |
| Amlodipine | Calcium channel blocker | Ankle swelling, flushing, headache | Older adults, African/Caribbean descent, isolated systolic hypertension | None | £3-£7/month |
| Hydrochlorothiazide | Diuretic | Low potassium, frequent urination, dizziness | Mild hypertension, older adults, combo therapy | None | £1-£4/month |
| Valsartan | ARB | Dizziness, fatigue, stomach upset | Post-heart attack, heart failure, ACE intolerance | Low (under 5%) | £5-£10/month |
| Ramipril | ACE inhibitor | Dry cough, dizziness, high potassium | Heart failure, post-heart attack | High (up to 20%) | £3-£7/month |
Which Alternative Is Right for You?
There’s no one-size-fits-all answer. But here’s how to think about it:
- If you have a dry cough → Switch to losartan or valsartan. ARBs are your best bet.
- If you’re over 55 or of African/Caribbean descent → Amlodipine or HCTZ often work better than ACE inhibitors.
- If you have heart failure or had a heart attack → Ramipril or valsartan may be preferred over lisinopril.
- If your blood pressure is only slightly high → HCTZ alone might be enough, and it’s the cheapest option.
- If you’re diabetic with kidney disease → Losartan or lisinopril are both good-but if you can’t tolerate lisinopril, losartan is the next best.
Don’t switch on your own. Always talk to your GP or pharmacist. They’ll check your kidney function, potassium levels, and other meds you’re taking before making a change.
What to Expect When Switching
Switching from lisinopril to another drug doesn’t happen overnight. Your doctor will usually:
- Check your blood pressure, kidney function, and potassium levels before switching
- Start you on a low dose of the new drug
- Wait 2-4 weeks to see how you respond
- Adjust the dose if needed
- Re-check your blood pressure and labs after 6 weeks
Some people feel better within days. Others take weeks. Don’t panic if your pressure fluctuates a bit-it’s normal while your body adjusts.
When NOT to Switch
There are times when staying on lisinopril makes sense:
- You’re pregnant or planning to be-ACE inhibitors can harm a developing baby. Switch to methyldopa or labetalol instead.
- You’ve been on it for years and it’s working perfectly with no side effects.
- You have a history of angioedema (swelling under the skin)-this can happen with ACE inhibitors and ARBs, so you may need a different class entirely.
- You’re on multiple meds for heart failure-your doctor may have chosen lisinopril for a specific reason.

Real-Life Scenarios
Here are two common cases I’ve seen in clinics in Leeds:
Case 1: Maria, 68, has been on lisinopril for 5 years. She’s got a dry cough that keeps her up at night. Her blood pressure is fine, but the cough is driving her crazy. Her GP switches her to losartan. Within 10 days, the cough is gone. Her BP stays steady. She’s thrilled.
Case 2: James, 72, of Jamaican descent. His blood pressure stays high even on lisinopril. His doctor tries increasing the dose-it helps a little, but not enough. Then they switch to amlodipine. His pressure drops into the target range, and he feels more energetic. No cough, no swelling. Perfect fit.
Final Thoughts
Hypernil (lisinopril) is a solid, well-tested drug. But it’s not the only option-and it’s not always the best one for you. If you’re struggling with side effects or your blood pressure isn’t where it should be, talk to your doctor. There are other pills out there that might work better, with fewer problems.
Don’t suffer in silence. Your blood pressure matters. Your comfort matters. And there’s no shame in asking for a change.
Is Hypernil the same as lisinopril?
Yes. Hypernil is a brand name for the generic drug lisinopril. They contain the same active ingredient, work the same way, and have the same side effects. The only difference is the manufacturer and the price-generic lisinopril is usually cheaper.
Can I switch from lisinopril to losartan on my own?
No. Never switch blood pressure medications without your doctor’s guidance. Stopping or changing suddenly can cause dangerous spikes in blood pressure. Your doctor will monitor your kidney function and potassium levels before and after the switch to make sure it’s safe.
Which alternative has the least side effects?
Hydrochlorothiazide and amlodipine generally have fewer systemic side effects than ACE inhibitors. Neither causes the dry cough linked to lisinopril. However, amlodipine can cause swollen ankles, and HCTZ can lower potassium. The "least side effects" depends on your body-what’s mild for one person can be bothersome for another.
How long does it take for a new blood pressure pill to work?
Most blood pressure meds start working within a few days, but it can take 2 to 6 weeks to reach their full effect. Your doctor will usually wait 4-6 weeks before deciding if the new drug is working well enough. Don’t stop or change the dose just because you don’t feel different right away.
Are natural alternatives like garlic or magnesium safe instead of lisinopril?
Supplements like garlic, magnesium, or hibiscus tea may help lower blood pressure a little-but they are not replacements for prescribed medication. If you’re on lisinopril for a reason (like heart failure or kidney protection), stopping it for supplements can be dangerous. Always talk to your doctor before adding supplements, as they can interact with your meds.
Can I take lisinopril and amlodipine together?
Yes. In fact, it’s very common. Many people need more than one drug to control their blood pressure. Lisinopril and amlodipine work in different ways, so they’re often combined for better results. This combo is widely used and well-studied in guidelines from the British Hypertension Society.
Next Steps
If you’re thinking about switching from Hypernil:
- Write down your symptoms-cough, dizziness, swelling, fatigue
- Check your latest blood pressure readings
- Make a list of all other medications and supplements you take
- Book an appointment with your GP or practice nurse
- Ask: "Is there a better option for me based on my health and side effects?"
There’s no rush. But if your current medication isn’t working-or is making you feel worse-it’s worth having the conversation. You deserve to feel well, not just to have a number on a chart that’s "normal."
Andy Slack
November 3, 2025 AT 17:21Just switched from lisinopril to losartan last month after 3 years of that damn cough. Gone in 4 days. No more waking up like I’m choking on a dust bunny. Life is quiet again. Also, my BP’s actually lower now. Who knew?
Rashmi Mohapatra
November 4, 2025 AT 22:12bro lisinopril made me feel like a zombie and my ankles looked like balloons. switched to amlodipine and now i feel like i can run a marathon… if i wanted to. also no cough. no more sneezing at my own shadow. thank u god for calcium channel blockers
Ryan Masuga
November 5, 2025 AT 06:13Hey, if you’re on lisinopril and it’s working fine-keep it. But if you’re struggling, don’t feel guilty for asking for a change. Your body isn’t broken, it’s just telling you it needs something else. I’ve seen people go from miserable to amazing just by switching to losartan or HCTZ. You’re not failing-you’re optimizing.
Jennifer Bedrosian
November 6, 2025 AT 06:10OMG I CAN’T BELIEVE PEOPLE STILL TAKE LISINOPRIL LIKE IT’S A LIFESTYLE CHOICE 😭 my doc tried to give me that and I said NOPE not today Satan. switched to amlodipine and now I don’t feel like I’m slowly turning into a human cough drop. also my feet don’t look like overinflated beach balls anymore. #NoMoreCough #AmlodipineIsMySavior
Lashonda Rene
November 6, 2025 AT 06:42So I’ve been on lisinopril for 8 years and honestly I never had a problem until I started getting dizzy every time I stood up. I didn’t think much of it until my mom said hey maybe it’s the med. So I went to my doc and we tried hydrochlorothiazide and it was like night and day. No cough, no dizziness, just me being me again. I know some people say it lowers potassium but I just eat bananas and it’s fine. I’m not a doctor but if you’re feeling off maybe talk to your doc about it? It’s not a big deal to switch, really.
Kelsey Veg
November 6, 2025 AT 10:28Everyone’s acting like switching meds is some revolutionary act. It’s not. Lisinopril is a 1980s drug with a 20% cough rate. The fact that people still tolerate it like it’s a virtue is just sad. Amlodipine and ARBs have been gold standard for decades. If your doc pushes lisinopril without asking about side effects, they’re lazy. Not you. Your doc.
Alex Harrison
November 7, 2025 AT 17:17Just wanted to say thanks for the table. I printed it out and took it to my appt. Doc was like wow you did your homework. We switched me to valsartan and I’ve been good for 3 weeks now. No cough, no swelling, just chill. I didn’t know ARBs were that different from ACEs. Learned something today.
Jay Wallace
November 8, 2025 AT 19:49Listen, if you’re American and you’re taking a British brand name like Hypernil, you’re already doing it wrong. Get the generic. Lisinopril is $3 a month at Walmart. Losartan? $4. Why are you paying for marketing? This isn’t luxury skincare. This is medicine. Stop being a sucker.
Alyssa Fisher
November 9, 2025 AT 01:05It’s interesting how we treat blood pressure meds like they’re interchangeable tools, when in reality they’re deeply biological interventions. ACE inhibitors affect the renin-angiotensin system, which is tied to inflammation, kidney perfusion, even emotional regulation. The dry cough isn’t just a side effect-it’s a signal. The fact that we’ve normalized it for decades says more about medical inertia than patient tolerance. Switching isn’t weakness. It’s listening.
Alyssa Salazar
November 10, 2025 AT 23:58For anyone considering HCTZ-don’t. It’s a band-aid. It lowers BP by dehydrating you, which sounds great until your electrolytes go haywire and you get muscle cramps at 3am. ARBs and CCBs are superior because they target vascular tone, not fluid volume. HCTZ is for elderly patients with isolated systolic HTN and zero comorbidities. If you’re diabetic, have CKD, or are under 65-don’t start there. The data is clear. This isn’t opinion. It’s guideline-based practice.