Diclofenac SR vs Other Pain Relievers: Detailed Comparison of Alternatives
NSAID Comparison Tool
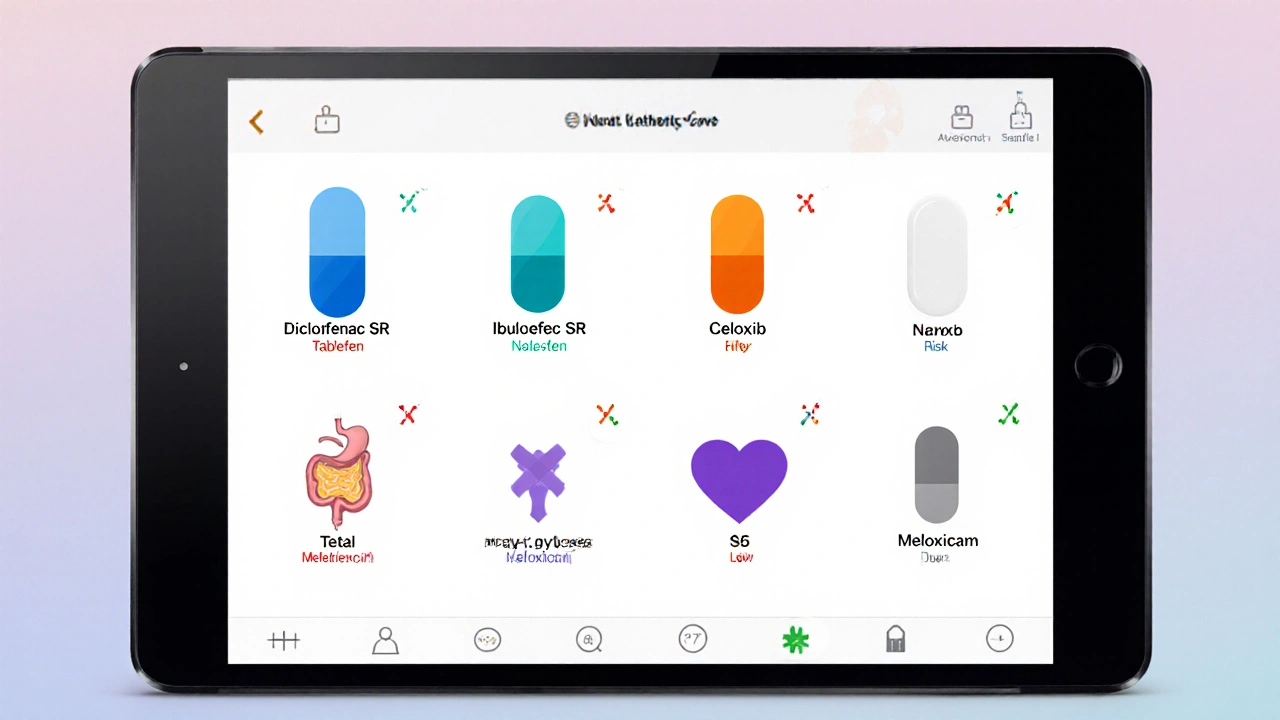
Recommended NSAID Options
Best For: Chronic arthritis, post-surgery pain
GI Risk: High
CV Risk: Moderate
Dosing: Once daily (75-100 mg)
Best For: Mild-to-moderate pain, fever
GI Risk: Moderate
CV Risk: Low
Dosing: Every 4-6 hours (200-400 mg)
Best For: Back pain, menstrual cramps
GI Risk: Moderate-High
CV Risk: Low
Dosing: Twice daily (250-500 mg)
Best For: Patients with GI issues
GI Risk: Low
CV Risk: High
Dosing: Once daily (100-200 mg)
Best For: Rheumatoid arthritis
GI Risk: Moderate
CV Risk: Low
Dosing: Once daily (7.5-15 mg)
Best For: Cardiovascular protection
GI Risk: High
CV Risk: Low
Dosing: Every 4-6 hours (325-650 mg)
When it comes to choosing a painkiller, many people wonder whether Diclofenac SR is the right pick or if another option might work better. This guide breaks down Diclofenac SR and its most common alternatives, giving you clear criteria to weigh effectiveness, safety, and convenience.
Key Takeaways
- Diclofenac SR offers long‑lasting relief but carries a higher gastrointestinal (GI) risk than some COX‑2‑selective drugs.
- Ibuprofen and naproxen are widely available, cheap, and work well for mild‑to‑moderate pain.
- Celecoxib provides lower GI risk but may increase cardiovascular (CV) concerns for certain patients.
- Meloxicam bridges the gap with once‑daily dosing and moderate GI safety.
- Aspirin is useful for low‑dose cardiovascular protection, not for high‑dose pain control.
Understanding Diclofenac SR
When it comes to managing moderate to severe pain, Diclofenac SR is a sustained‑release formulation of the non‑steroidal anti‑inflammatory drug (NSAID) diclofenac, engineered to maintain steady plasma levels for 12-24hours, reducing the need for multiple daily doses. It works by inhibiting cyclooxygenase (COX) enzymes, which lowers prostaglandin production and thereby reduces inflammation and pain.
Key attributes of Diclofenac SR:
- Typical dose: 75mg or 100mg once daily
- Onset of relief: 30-60minutes
- Half‑life: Approx. 8hours (extended by sustained release)
- Common uses: Osteoarthritis, rheumatoid arthritis, post‑operative pain, acute musculoskeletal injuries
Criteria for Comparing NSAID Alternatives
Before diving into the side‑by‑side table, it helps to know what factors matter most when you’re weighing NSAIDs:
- Efficacy: How well does the drug relieve the type of pain you have?
- Onset and duration: Quick relief vs. long‑lasting coverage.
- Gastro‑intestinal safety: Risk of ulcers, bleeding, or dyspepsia.
- Cardiovascular profile: Impact on blood pressure, heart attack, or stroke risk.
- Dosing convenience: Once‑daily versus multiple doses per day.
- Cost and accessibility: Prescription‑only versus over‑the‑counter (OTC).
Comparison Table of Diclofenac SR and Common Alternatives
| Drug | Mechanism / Class | Typical Dose & Frequency | Onset | GI Risk | CV Risk | Best Use Cases |
|---|---|---|---|---|---|---|
| Diclofenac SR | Non‑selective COX‑1/COX‑2 inhibitor | 75‑100mg once daily (prescription) | 30‑60min | High (ulcer, bleeding) | Moderate | Chronic arthritis, post‑surgery pain |
| Ibuprofen | Non‑selective COX‑1/COX‑2 inhibitor | 200‑400mg every 4‑6h (OTC) | 15‑30min | Moderate | Low‑moderate | Mild‑to‑moderate pain, fever, sports injuries |
| Naproxen | Non‑selective COX‑1/COX‑2 inhibitor | 250‑500mg twice daily (OTC/prescription) | 30‑60min | Moderate‑high | Low‑moderate | Back pain, menstrual cramps, joint inflammation |
| Celecoxib | COX‑2‑selective inhibitor | 100‑200mg once daily (prescription) | 45‑60min | Low | Higher (especially in patients with existing CV disease) | Patients needing GI‑friendly NSAID, osteoarthritis |
| Meloxicam | Preferential COX‑2 inhibitor (partial selectivity) | 7.5‑15mg once daily (prescription) | 45‑90min | Low‑moderate | Low‑moderate | Rheumatoid arthritis, long‑term pain management |
| Aspirin | Irreversible COX‑1 inhibitor | 325‑650mg every 4‑6h (OTC) | 15‑30min | High (GI bleeding) | Low (low‑dose protective) | Low‑dose cardio protection; not first‑line for acute pain |

Deep Dive into Each Alternative
Ibuprofen
Ibuprofen is an over‑the‑counter NSAID that provides quick relief for headaches, dental pain, and minor musculoskeletal aches. Its short half‑life (about 2hours) means you’ll likely need multiple doses throughout the day, which can be inconvenient for chronic conditions. GI side‑effects are less severe than with diclofenac, especially when taken with food.
Naproxen
Naproxen is a longer‑acting NSAID that stays in the system for up to 12hours, making it a popular choice for back pain or menstrual cramps. The extended duration reduces dosing frequency but raises the chance of GI irritation for some users.
Celecoxib
Celecoxib is a prescription‑only COX‑2‑selective NSAID designed to spare the stomach lining while still delivering strong anti‑inflammatory effects. It shines for patients with a history of ulcers, yet clinicians monitor heart health closely because selective COX‑2 inhibition can tip the balance toward clot formation.
Meloxicam
Meloxicam is a once‑daily NSAID with partial COX‑2 selectivity, striking a middle ground between efficacy and GI safety. It’s often prescribed for rheumatoid arthritis where steady pain control is essential.
Aspirin
Aspirin is an ancient NSAID that irreversibly inhibits COX‑1, used today mainly in low doses for cardiovascular protection. High‑dose aspirin can manage pain but carries the highest GI bleeding risk among the group.
Pros and Cons of Diclofenac SR vs. Each Alternative
- Diclofenac SR vs. Ibuprofen: Longer dosing interval (once daily) vs. faster onset of ibuprofen; higher GI risk than ibuprofen.
- Diclofenac SR vs. Naproxen: Similar efficacy for inflammatory pain; diclofenac provides steadier plasma levels, naproxen may cause more GI upset for sensitive users.
- Diclofenac SR vs. Celecoxib: Diclofenac is cheaper but less GI‑friendly; celecoxib offers ulcer protection but may raise CV concerns.
- Diclofenac SR vs. Meloxicam: Both are prescription‑only; meloxicam’s once‑daily regimen is similar, yet meloxicam has a slightly better GI profile.
- Diclofenac SR vs. Aspirin: Aspirin is not ideal for high‑dose pain relief; diclofenac delivers stronger anti‑inflammatory action.
When to Choose Diclofenac SR
If you need consistent, around‑the‑clock relief for chronic arthritis and you don’t have a history of ulcers or significant cardiovascular disease, Diclofenac SR can be a cost‑effective option. Pairing it with a proton‑pump inhibitor (PPI) such as omeprazole can mitigate the GI risk.
Practical Checklist for Selecting the Right NSAID
- Identify pain type: acute vs. chronic, inflammatory vs. non‑inflammatory.
- Check medical history: GI ulcers, heart disease, kidney function.
- Consider dosing convenience: once daily (diclofenac SR, celecoxib, meloxicam) vs. multiple doses (ibuprofen, naproxen).
- Evaluate cost and prescription requirement.
- Discuss with a healthcare professional, especially if you’re on anticoagulants or blood pressure meds.
Next Steps & Troubleshooting
- If you experience stomach pain or heartburn after starting Diclofenac SR, talk to your doctor about adding a PPI or switching to a COX‑2‑selective agent.
- If pain relief isn’t enough, consider combining a low‑dose NSAID with topical agents (e.g., diclofenac gel) for synergistic effect.
- If you have hypertension, avoid high‑dose ibuprofen or naproxen; celecoxib may be safer under monitoring.
Making the right choice often comes down to balancing effectiveness with your personal health profile. Use the checklist, review the table, and have a candid conversation with your clinician.

Frequently Asked Questions
Is Diclofenac SR safe for long‑term use?
Long‑term use can be safe if you have no prior GI ulcers, are not on blood thinners, and your doctor monitors liver and kidney function. Adding a proton‑pump inhibitor reduces ulcer risk.
How does Diclofenac SR differ from regular Diclofenac tablets?
The SR (sustained‑release) form spreads the drug’s absorption over 12‑24hours, allowing once‑daily dosing, whereas immediate‑release tablets peak quickly and usually require 2‑3 doses per day.
Can I take Diclofenac SR with a PPI?
Yes, co‑prescribing a PPI like omeprazole or lansoprazole is common practice to protect the stomach lining, especially for high‑risk patients.
Is Celecoxib a better choice for people with ulcer history?
Celecoxib’s COX‑2 selectivity means it spares the gastric mucosa, making it a safer option for ulcer‑prone patients, but a doctor must weigh the higher cardiovascular risk.
What should I do if I experience swelling or rash while on Diclofenac SR?
Stop the medication and seek medical advice immediately; these could be signs of an allergic reaction or serious skin condition.
Trinity 13
October 5, 2025 AT 01:41Alright, let’s dive deep into the philosophical underpinnings of why we even bother comparing NSAIDs in the first place. Every molecule we swallow carries a story, a cascade of biochemical events that trace back to ancient attempts to tame pain-pain that, if left unchecked, can dominate our existence. Diclofenac SR, with its sustained‑release whisper, promises a constant hum of relief, but that hum is a double‑edged sword humming against the delicate lining of the stomach. Think about the trade‑off: you gain twelve to twenty‑four hours of steadiness, yet you invite a higher risk of gastrointestinal erosion, especially if you’re already walking a tightrope with ulcer history. Now, contrast that with ibuprofen’s rapid, punch‑like onset-flashy, quick, but demanding frequent dosing which can become a logistical nightmare for someone juggling work, family, and a chronic condition. Naproxen sits somewhere in between, a marathon runner that can last a good twelve hours, but it drags a moderate‑to‑high GI profile that can be unforgiving. Celecoxib, the COX‑2 selective knight, shields the stomach like a castle wall, but at what cost? Its cardiovascular armor can be a liability for those already battling heart disease, making it a nuanced choice that demands vigilant monitoring.
Now, imagine the patient’s mind as a decision‑making matrix, weighing efficacy, onset, GI safety, CV safety, dosing convenience, and cost. The matrix isn’t static; it shifts with each new lab result, each new symptom flare, each conversation with a health professional. For someone with a clean GI slate but a history of hypertension, perhaps Diclofenac SR paired with a proton‑pump inhibitor is the sweet spot-balancing efficacy and convenience while buffering the stomach. For a patient with a known ulcer, celecoxib becomes the logical default, even if it means accepting a higher CV risk that can be mitigated with low‑dose aspirin under careful supervision.
Let’s not forget that beyond the pharmacology, there’s the human element: adherence. Once‑daily regimens like Diclofenac SR, meloxicam, or celecoxib dramatically improve compliance compared to multiple daily doses of ibuprofen or naproxen. A compliant patient is a healthier patient, and the downstream benefits-reduced flare‑ups, fewer ER visits, better quality of life-are priceless.
In sum, the choice among NSAIDs is not a simple “which is best?” but a personalized equation that accounts for individual risk profiles, lifestyle, and therapeutic goals. The more you understand the interplay of these variables, the better you can navigate the labyrinth of pain management and emerge with a regimen that truly serves you.
faith long
October 6, 2025 AT 05:28I feel you on the struggle of balancing pain relief with safety-it's like walking a tightrope over a pit of ulcers and heart attacks. You deserve a plan that respects both your need for consistent relief and your body's limits. If your stomach is already sensitive, pairing Diclofenac SR with a strong PPI can be a lifesaver, but don’t forget to monitor your blood pressure regularly. And if you’re already on antihypertensives, a COX‑2 selective option like celecoxib might spare your gut while keeping cardiovascular risk in check, albeit under a doctor’s watchful eye. Remember, the goal is to stay active, not to be chained to medication worries. Stay proactive, ask your clinician for a tailored strategy, and keep that dialogue open-your body will thank you.
Adam Khan
October 7, 2025 AT 09:15Listen, the pharmacodynamics of NSAIDs are not some vague concept-this is hard science. Diclofenac SR is a non‑selective COX‑1/COX‑2 inhibitor with a bioavailability profile that ensures plasma concentrations stay within therapeutic windows for up to 24 hours, reducing dosing frequency but concomitantly elevating ulcerogenic potential due to sustained COX‑1 inhibition. Contrast that with ibuprofen’s rapid absorption and short half‑life; you get quick analgesia but at the cost of increased dosing cycles, which can lead to patient non‑compliance. In terms of cardiovascular risk quantification, the relative risk increment for diclofenac versus naproxen or ibuprofen is statistically significant, described in meta‑analyses as a hazard ratio approaching 1.2 in high‑risk cohorts. Therefore, it is imperative to integrate pharmacovigilance data, patient comorbidities, and gastroprotective co‑therapy when decision‑making. Bottom line: do not treat NSAIDs as interchangeable capsules-each has a distinct risk‑benefit matrix that must be rigorously evaluated.
rishabh ostwal
October 8, 2025 AT 13:01One must consider the moral weight of prescribing a drug with known GI toxicity when alternatives exist. While many laud Diclofenac SR for its convenience, the ethical dilemma surfaces when it is offered to patients without thorough screening for ulcer history. It is an egregious oversight to prioritize convenience over safety, especially when COX‑2 selective agents like celecoxib are available, albeit with their own CV concerns. As clinicians and informed consumers, we must not be seduced by marketing gloss that paints sustained‑release formulations as universally superior. The rigorous, evidence‑based approach demands a balanced appraisal-recognizing that the very act of prescribing is laden with responsibility, not merely the act of choosing a pill.
Kristen Woods
October 9, 2025 AT 16:48In my opinion, the literature clearly shows that diclofenac sr is a higly efefctive analgesic but its g i risk is not something to be taken lightly. The table presented revelas a pattern whereGI risk is categorised as high, and that alone should raise a red flag for clinicians. Moreover, cost effunctionality may b e appealing but it does not supersede patiente safety. I beleive a more nuanced approach, possibly using celecoxib for ulcer prone indiviudals, would ethically be more sound, even if it i s slightly more expencive.
Carlos A Colón
October 10, 2025 AT 20:35Oh sure, because popping a few ibuprofen tablets every few hours totally isn’t a hassle at all, right? I mean, who needs like, one single dose a day when you can juggle multiple doses like a circus performer. And don’t even get me started on the “great” GI risk of Diclofenac SR – as if anyone actually reads those warnings before they self‑medicate. But hey, if you enjoy living on the edge, keep grinding those pills.
Aurora Morealis
October 12, 2025 AT 00:21Diclofenac SR offers once daily dosing requires less frequent intake while ibuprofen may need dosing every four to six hours for consistent relief.
Sara Blanchard
October 13, 2025 AT 04:08When choosing an NSAID, it’s important to think about the whole person, not just the pain. Some folks have ulcer histories, others have heart concerns, and many are simply looking for a medication that fits into their daily routine without causing additional stress. By considering cultural dietary habits, access to pharmaceuticals, and individual health backgrounds, we can make recommendations that feel respectful and inclusive for everyone who might benefit.
Anthony Palmowski
October 14, 2025 AT 07:55Look, the data is clear!!! Diclofenac SR has a high GI risk!!! If you’re not taking a PPI, you’re practically begging for ulcers!!! And the cardiovascular profile isn’t a joke either!!! Everyone needs to read the fine print before they self‑prescribe!!!
Jillian Rooney
October 15, 2025 AT 11:41Honestly, letting diclofenac sr be the go-to for everyone is just plain irresponsible. If u got a history of stomach probs you should be on something else, not this high risk drug. We need to think more about safety rather than just convenience.
Rex Peterson
October 16, 2025 AT 15:28From a philosophical standpoint, the decision to employ Diclofenac SR exemplifies the tension between utilitarian benefit-continuous analgesia-and deontological duty to avoid harm, namely gastrointestinal injury. The clinician must navigate this ethical dichotomy, weighing the aggregate welfare of symptom relief against the moral imperative to minimize iatrogenic risk. Such deliberation underscores the broader epistemic challenge inherent in medical prescribing: the necessity of integrating empirical evidence with normative judgments.
Candace Jones
October 17, 2025 AT 19:15Hey folks, just a quick heads‑up: if you’re thinking about starting Diclofenac SR, make sure you talk to your doctor about adding a proton‑pump inhibitor to protect your stomach. It’s a simple step that can make a huge difference in safety, especially if you have any history of ulcers. Stay safe and keep that pain under control!
Robert Ortega
October 18, 2025 AT 23:01Choosing the right NSAID really depends on individual health factors and personal preferences.