Holistic Psoriasis Management: Why a Whole‑Body Approach Matters
Psoriasis Management Plan Builder
Create Your Personalized Psoriasis Management Plan
Enter your current situation to get tailored recommendations for improving your psoriasis management.
Key Takeaways
- Psoriasis flares are influenced by skin care, lifestyle, mental health, and comorbidities.
- A holistic plan blends medical therapy with diet, exercise, stress control, and patient education.
- Regular screening for heart disease, diabetes, and depression can prevent serious complications.
- Personalized goals and a simple tracking checklist keep treatment on track.
- Small, sustainable changes often outperform aggressive, short‑term fixes.
Living with psoriasis can feel like a constant juggling act-prescriptions, itchy patches, awkward social moments, and the fear of flare‑ups. Most people try a cream or two and hope for the best, only to discover that the skin symptoms return when stress spikes or a favorite snack is missed. The missing piece is a holistic approach that treats the whole person, not just the rash. Below you’ll learn how to build a plan that combines proven medical treatments with everyday habits, so the skin improves and you feel better overall.
What Is Psoriasis?
Psoriasis is a chronic autoimmune condition where skin cells grow 10 times faster than normal, causing red, scaly plaques. Around 2-3% of the global population lives with the disease, and its severity can range from a few isolated patches to widespread involvement that affects quality of life. Common triggers include skin injury, infections, certain medications, and lifestyle factors such as alcohol, smoking, and stress. Because the immune system is involved, psoriasis often coexists with other health issues like heart disease, type‑2 diabetes, and depression.
Why a Holistic Approach Works
Traditional care focuses on suppressing inflammation with topical steroids, systemic drugs, or UV light. While these therapies are essential, they don’t address the underlying lifestyle and emotional contributors that drive flares. A holistic model looks at five interconnected pillars: medical treatment, skin‑care routine, nutrition, mental‑well‑being, and comorbidity management. By aligning all five, patients experience fewer break‑outs, reduced medication dosages, and better overall health.
Core Pillars of Holistic Management
- Evidence‑Based Medical Therapy - topical, systemic, or phototherapy as prescribed by a dermatologist.
- Skin‑Care Routine - gentle cleansing, moisturisation, and barrier repair.
- Nutrition & Lifestyle - anti‑inflammatory foods, regular exercise, weight control.
- Mental Health Support - stress‑reduction techniques, counseling, sleep hygiene.
- Comorbidity Screening - cardiovascular risk, diabetes, depression checks.

Integrating Conventional Treatments
When it comes to medication, three main options dominate:
- Topical therapy (corticosteroids, vitamin D analogues, calcineurin inhibitors) works best for mild‑to‑moderate patches. Apply thinly once or twice daily, and rotate strengths to minimise skin thinning.
- Systemic therapy includes biologics (TNF‑α inhibitors, IL‑17 blockers) and oral agents like methotrexate or apremilast. These are reserved for moderate‑to‑severe disease or when topical options fail.
- Phototherapy (narrow‑band UVB or excimer laser) can clear plaques within weeks, especially for patients who cannot tolerate systemic drugs.
Choosing the right regimen depends on plaque location, severity score (e.g., PASI), lifestyle, and personal preference. Regular follow‑up appointments allow the dermatologist to adjust dosage, rotate medications, and monitor side effects.
Lifestyle Strategies That Complement Medicine
Research from the National Psoriasis Foundation (2023) shows that a diet low in saturated fat and high in omega‑3 fatty acids can reduce the PASI score by up to 15% when combined with standard therapy. Here’s how to incorporate evidence‑backed habits:
- Diet: Emphasise leafy greens, berries, fatty fish, and whole grains. Limit processed meats, sugary drinks, and excessive alcohol.
- Exercise: Aim for 150 minutes of moderate aerobic activity weekly. Weight loss of just 5% can markedly improve plaque thickness in overweight patients.
- Stress management: Mindfulness meditation, yoga, or even a daily 10‑minute breathing routine reduces cortisol spikes that often trigger flares.
- Sleep hygiene: 7-9 hours per night supports immune regulation. Dark, cool bedroom environments help keep skin moisture balanced.
Building Your Personal Management Plan
- Set Clear Goals - Decide whether you aim to reduce plaque size, prevent new lesions, or lower medication dosage.
- Document Baseline - Take photos of affected areas, note PASI score (if available), and record any comorbid symptoms.
- Choose Core Treatments - Work with your dermatologist to select a medical regimen that fits your severity and lifestyle.
- Create a Daily Skin‑Care Routine - Use a fragrance‑free cleanser, apply a ceramide‑rich moisturizer within three minutes of showering, and re‑moisturise every 4-6hours.
- Integrate Lifestyle Choices - Add two servings of oily fish per week, schedule three 30‑minute walks, and block 10 minutes for meditation each morning.
- Monitor Comorbidities - Quarterly blood pressure checks, annual HbA1c test, and mental‑health screening questionnaires.
- Review and Adjust - Every 3 months, assess what worked, capture flare triggers, and tweak medication or habits accordingly.
Keep a simple spreadsheet or a phone app to log skin condition, stress levels, diet, and medication use. Patterns often emerge that reveal hidden triggers.
Common Pitfalls & Pro Tips
- Skipping Moisturiser - Even on “good” days, dry skin invites irritation and reduces drug absorption.
- Over‑reliance on Steroids - Long‑term high‑potency steroids can cause skin atrophy; rotate with non‑steroidal topicals when possible.
- Ignoring Mental Health - Untreated depression or anxiety raises inflammatory markers and worsens plaques.
- Neglecting Comorbid Checks - Cardiovascular disease risk is 1.5‑2× higher in psoriasis; regular labs can catch problems early.
- All‑Or‑Nothing Diets - Extreme restrictions lead to burnout. Aim for modest, sustainable changes instead of fad plans.
Pro tip: Pair any new medication with a consistent moisturiser routine; the skin barrier improves drug penetration, meaning you may need a lower dose.
Comparison of Main Treatment Modalities
| Aspect | Topical Therapy | Systemic Therapy | Phototherapy |
|---|---|---|---|
| Typical Use | Mild‑to‑moderate plaques | Moderate‑to‑severe or resistant disease | Widespread involvement, pregnancy‑compatible option |
| Onset of Improvement | 2‑4 weeks | 4‑12 weeks (varies by biologic) | 1‑3 weeks |
| Side‑Effect Profile | Skin thinning, irritation | Infection risk, liver toxicity, lipid changes | Skin aging, rare burns |
| Administration | Topical application | Injection or oral tablet | Clinic‑based UV sessions 2‑3×/week |
| Cost (US‑2025) | $10‑$50 per month | $1,200‑$3,200 per year (biologics) | $150‑$300 per course |
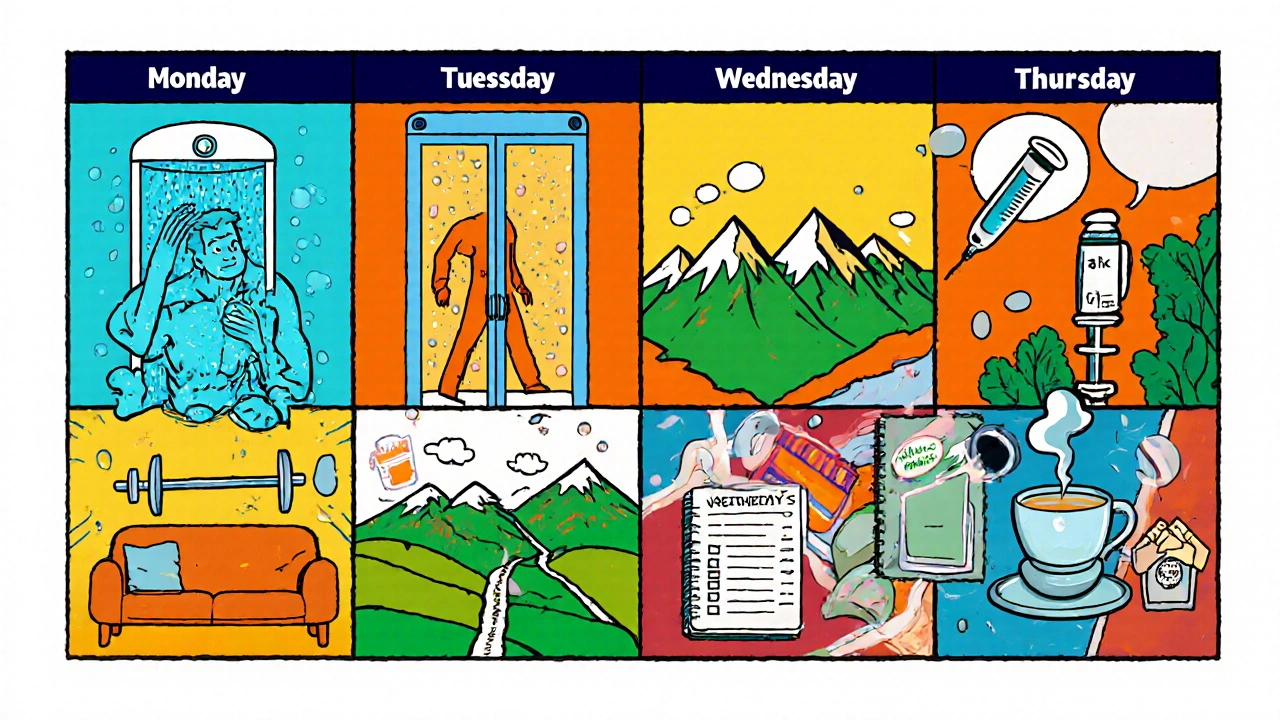
Putting It All Together: A Sample Week
Below is a realistic snapshot of a balanced plan for an adult with moderate plaque psoriasis.
- Monday: Apply prescribed vitamin D cream after shower; 30‑minute brisk walk; 10‑minute guided meditation before bed.
- Tuesday: Attend phototherapy session; prepare salmon salad for lunch (rich in omega‑3); log stress level (scale 1‑10).
- Wednesday: Switch to low‑potency steroid on elbows; strength‑training (bodyweight); check blood pressure.
- Thursday: Bio‑logical injection (if on biologic); swap coffee for green tea; 15‑minute stretching before work.
- Friday: Gentle cleanser + ceramide moisturizer; weekend hike; family dinner with whole‑grain pasta.
- Saturday: Review photo journal; plan grocery list (avoid processed snacks); early bedtime.
- Sunday: Rest day - focus on hobbies; reflect on mood journal; prepare medication for the upcoming week.
Notice how each day mixes medical action, skin care, movement, and mental‑wellness. That rhythm builds resilience against flares.
Frequently Asked Questions
Can diet really affect psoriasis severity?
Yes. Studies show that a diet high in omega‑3 fatty acids, fiber, and antioxidants can lower inflammatory markers. Cutting down on red meat, sugary drinks, and excessive alcohol often translates into smaller, less itchy plaques.
Do I need to see a dermatologist if my patches are small?
Even mild psoriasis benefits from professional guidance. A dermatologist can confirm the diagnosis, recommend appropriate topical agents, and screen for hidden comorbidities that often accompany the condition.
Is phototherapy safe for long‑term use?
When administered under medical supervision, narrow‑band UVB phototherapy is considered safe for most patients. Risks include premature skin aging and a slight increase in skin‑cancer risk, which is mitigated by regular skin checks.
How often should I screen for heart disease?
Adults with psoriasis should have cholesterol, blood pressure, and fasting glucose measured at least once a year. If you have additional risk factors (smoking, obesity), discuss more frequent testing with your GP.
Can stress‑relief techniques replace medication?
Stress management alone rarely cures psoriasis, but it can lower flare frequency and may allow lower medication doses. Think of it as a complementary tool rather than a substitute.
Laura Barney
October 15, 2025 AT 21:09I love how this guide stitches together med‑talk and day‑to‑day hacks – it feels like a recipe that actually tastes good. The pill‑and‑cream combo gets a bright side when you toss in a walk or a splash of omega‑3. I’ve tried the moisturizer‑after‑shower trick and the skin actually drinks the meds better. Keeping a simple spreadsheet is a genius move; I’ve seen my flare‑log shrink over a month. Overall, it’s a solid “whole‑you” playbook that feels doable.
Jessica H.
October 16, 2025 AT 22:09While the article is comprehensive, it lacks citations for several claims regarding dietary impact on PASI scores.
Tom Saa
October 17, 2025 AT 23:09The interplay between the immune cascade and lifestyle factors forms a tapestry that resists a simple linear explanation. When one pulls on the thread of stress, cortisol rises, and the keratinocyte turnover accelerates, echoing the biological narrative. Yet, the same thread, if rewoven with mindfulness, can dampen that response, suggesting a bidirectional pathway. The article correctly notes the prevalence of comorbidities, but it stops short of exploring the shared genetic loci that underlie both psoriasis and metabolic syndrome. A deeper dive into the IL‑23/Th17 axis would illuminate why certain biologics succeed where others falter. Moreover, the recommendation to log daily variables aligns with the principles of precision medicine, where data granularity informs therapeutic adjustments. However, the practical burden of maintaining a spreadsheet may deter patients already coping with symptom fatigue. In that light, a mobile app with automated prompts could serve as a less intrusive alternative. The nutritional advice emphasizes omega‑3 fatty acids, yet research also points to the role of vitamin D status in modulating immune activity. Incorporating safe sunlight exposure or supplementation could complement the dietary regimen. Exercise is presented as a weight‑control measure, but its anti‑inflammatory effects stem from myokine release, a nuance worth mentioning. Sleep hygiene, though briefly addressed, merits a more robust discussion given its impact on cytokine rhythms. The holistic framework proposed mirrors the emerging concept of “treat-to-target” beyond skin scores, aiming for cardiovascular and mental health endpoints as well. Ultimately, the success of such a multidimensional plan hinges on interdisciplinary collaboration among dermatologists, dietitians, and mental‑health professionals. In sum, the article offers a solid scaffold, but enriching it with mechanistic insights would elevate it from a practical checklist to a scientifically grounded roadmap.
John Magnus
October 19, 2025 AT 00:09From a mechanistic standpoint, the integration of biologic DMARDs with anti‑inflammatory nutritional protocols creates a synergistic downregulation of the NF‑κB signaling cascade, thereby attenuating keratinocyte hyperproliferation. Ignoring this axis in patient education is tantamount to prescribing a car with a full tank but no steering wheel. The proposed monitoring matrix should include CRP, lipid panels, and HOMA‑IR scores to truly capture systemic impact.
Marc Clarke
October 20, 2025 AT 01:09Looks solid, and I’m actually excited to try the weekly walk‑and‑meds combo. Small changes are the sweet spot, no need to overhaul life overnight.
angelica maria villadiego españa
October 21, 2025 AT 02:09I’ve been there; keeping a daily log helped me see patterns I never noticed before. Stick with it, and you’ll feel the difference.
Ted Whiteman
October 22, 2025 AT 03:09Wow, another ‘holistic’ hype train – but what if the diet part is just a marketing ploy? I still think the real magic lies in the right prescription, not kale smoothies.
Dustin Richards
October 23, 2025 AT 04:09Your point about stress management resonated with me; a few minutes of breathing really does calm the skin flare-ups. Keep sharing these practical tips.
Vivian Yeong
October 24, 2025 AT 05:09The checklist is useful, yet many patients will ignore it without proper coaching, rendering the plan ineffective.
suresh mishra
October 25, 2025 AT 06:09Include a brief note on UV‑B dosage safety; it prevents misuse.
Reynolds Boone
October 26, 2025 AT 06:09I’m curious about the suggested 150 minutes of aerobic activity – does intensity matter, or is any movement enough to see skin improvements?
Angelina Wong
October 27, 2025 AT 07:09You’ve got this! Pair your meds with a splash of salmon and a quick walk, and watch those plaques shrink. Consistency beats perfection any day.