How to Time Medication Doses to Reduce Infant Exposure During Breastfeeding

Many new mothers worry: can I take my medication and still breastfeed safely? The answer is yes-98% of medications are safe to use while nursing, as long as you time them right. It’s not about avoiding medicine altogether. It’s about working with your body’s natural rhythms to protect your baby while keeping yourself healthy.
Why Timing Matters More Than You Think
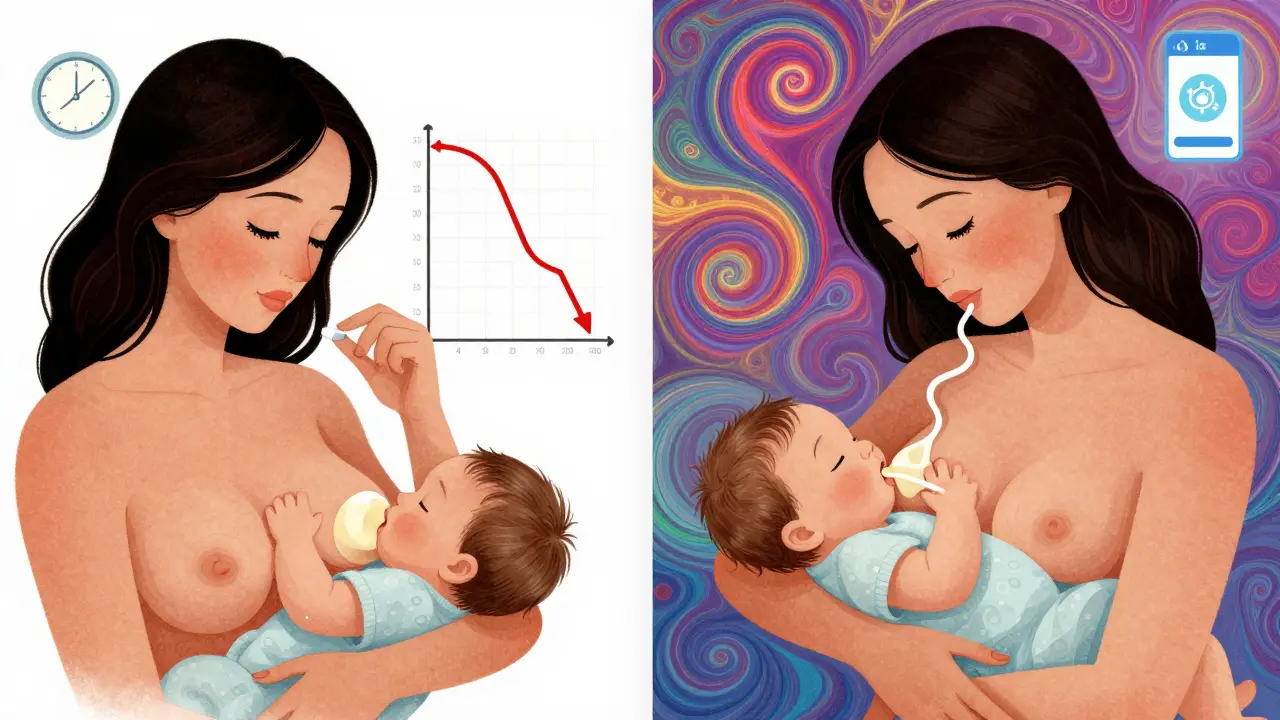
Medications don’t just sit in your bloodstream. They move into your breast milk, and your baby swallows them with every feed. But here’s the key: the amount of drug in your milk isn’t constant. It rises and falls based on when you took the pill, shot, or patch. Think of it like this: when you swallow a pill, your body absorbs it. Within minutes, it hits your bloodstream. Then, over the next hour or two, it peaks. That’s when the highest concentration flows into your milk. After that, your body starts breaking it down. By the time the drug’s level drops, so does what ends up in your milk. That’s why timing your dose around feedings makes a huge difference. If you take your medication right after nursing, your baby gets the lowest possible dose. By the next feed, much of the drug has cleared from your system.How to Time Your Doses: The Simple Rule
For most single-dose medications, the best practice is simple:- Feed your baby right before you take your medication.
- Wait as long as possible before the next feed.
- Hydrocodone (for pain): peaks in your blood at 0.5-2 hours, half-life of 3-4 hours. Take it after the longest stretch of sleep-usually after bedtime feeding.
- Oxycodone: peaks in 0.5-2 hours, half-life 3-4 hours. Same timing rule applies.
- Alprazolam (immediate-release): peaks in 1-2 hours, half-life 11 hours. Take after nursing, wait 4-6 hours before next feed.
What About Medications With Long Half-Lives?
Some drugs stick around for days. That’s where timing becomes less useful-and more risky.- Diazepam (Valium): half-life of 44-48 hours. Even if you time it perfectly, the drug builds up in your system. Infants can become overly sleepy or have trouble feeding.
- Fluoxetine (Prozac): half-life of 96 hours. Its active metabolite lasts over 260 hours. Experts at AAFP and ABM recommend avoiding it while breastfeeding if possible.
- Instead of diazepam: use lorazepam (half-life 10-20 hours, RID under 3%).
- Instead of fluoxetine: use sertraline (half-life 26 hours, RID under 1%).
- Instead of extended-release alprazolam: use immediate-release-it peaks faster and clears faster.
Steroids and Other Special Cases
Not all meds follow the same rules.- Prednisone: at standard doses, very little passes into milk. No need to delay feeding. But if you’re on a high dose (like 20 mg or more), wait 4 hours after taking it before nursing. That cuts exposure by over 80%.
- Birth control pills: combination pills (estrogen + progestin) can reduce milk supply. The AAFP recommends waiting at least 3-4 weeks after birth before starting them. Progestin-only pills are safer and can be started sooner.
- Antibiotics: most are fine. Penicillin, amoxicillin, cephalexin-all low risk. Just watch for signs of diaper rash or fussiness in your baby, which can signal a reaction to the medication.
What About Premature or Sick Babies?
Not all babies process drugs the same way.- Newborns under 2 weeks old have underdeveloped livers and kidneys. They clear drugs slowly.
- Premature babies? Even slower.
- Babies with kidney, liver, or neurological issues? Higher risk.
- Pump and dump after taking medication (especially for short-term, high-dose treatments like surgery pain meds).
- Use stored milk for the next 4-6 hours.
- Work with a lactation consultant to monitor for drowsiness, poor feeding, or weight loss.
Tools That Actually Help
You don’t have to remember all this on your own. There are trusted, free tools built for this exact purpose:- LactMed: a database from the National Library of Medicine. Updated monthly. Covers over 4,700 medications. Search by drug name, and it tells you peak time, half-life, RID, and whether to delay feeding.
- Hale’s Medication and Mothers’ Milk: the gold standard reference. Uses the Relative Infant Dose (RID) scale. Anything under 10% RID is generally safe. Many drugs are under 1%.
- LactMed app: free on iOS and Android. 127,000 active users as of 2023. You can save your meds, set reminders, and get alerts when your baby’s next feed is due.
What to Watch For in Your Baby
Even with perfect timing, watch for signs your baby might be reacting:- Unusual sleepiness or difficulty waking to feed
- Poor feeding or sucking
- Increased fussiness or irritability
- Changes in stool (diarrhea or constipation)
- Slower weight gain
Common Mistakes to Avoid
Even well-informed moms make these errors:- Taking meds right after feeding-this is the worst time. You’re handing your baby the peak dose.
- Assuming all SSRIs are the same-fluoxetine is risky. Sertraline and paroxetine are not.
- Using extended-release forms without checking-they’re harder to time and often unsafe for nursing.
- Stopping meds cold turkey-this can be dangerous for you. Talk to your doctor first.
- Waiting too long to ask for help-if you’re unsure, call a lactation consultant. Many NHS clinics offer free consultations.
When Timing Isn’t Enough
Sometimes, even the best timing won’t cut it. That’s when you need backup plans:- Pump and store milk before taking a high-risk or short-term med (like after surgery or a one-time antibiotic course).
- Use formula temporarily if your baby shows signs of reaction and you can’t switch meds.
- Ask your doctor about non-drug options-physical therapy for pain, CBT for anxiety, acupuncture for migraines.
By 4 to 6 weeks postpartum, your baby’s liver and kidneys are stronger. Their ability to process drugs improves. That’s why timing becomes easier-and more effective-as your baby grows.
Can I breastfeed after taking painkillers like ibuprofen or acetaminophen?
Yes. Both ibuprofen and acetaminophen are considered very safe during breastfeeding. They transfer in tiny amounts-less than 1% of your dose-and are cleared quickly. You don’t need to time these doses around feeds. They’re among the safest options for pain relief while nursing.
What if I need to take a medication that’s not recommended for breastfeeding?
Don’t panic. Many medications have safer alternatives. For example, if you’re on fluoxetine, your doctor can switch you to sertraline. If you need an opioid, hydrocodone is preferred over codeine. Always ask: "Is there a safer option?" Your healthcare provider should help you find one. If not, ask for a referral to a lactation specialist or maternal-fetal medicine expert.
Should I pump and dump after taking medication?
Only if the medication is high-risk and you can’t delay feeding or switch drugs. For most meds, pumping and dumping isn’t necessary. The drug clears from your system naturally. Pumping doesn’t speed that up. It just wastes milk. The exception is for short-term, high-dose meds like after surgery-then pumping before the dose and using stored milk for the next few hours is a smart strategy.
How do I know if a medication is safe while breastfeeding?
Check LactMed or Hale’s Medication and Mothers’ Milk. These are the most trusted sources. Avoid relying on drug labels-they often overstate risks. Most medications are safe. The key is knowing the half-life, peak time, and Relative Infant Dose (RID). If RID is under 10%, it’s generally safe. If you’re unsure, ask your pharmacist or a lactation consultant.
Can I breastfeed if I’m on antidepressants?
Yes, and many moms do. Sertraline and paroxetine are the top choices-they have low transfer rates and minimal side effects in infants. Fluoxetine and citalopram are riskier due to long half-lives. Timing helps, but switching to a safer drug is often better. Studies show over 90% of mothers on sertraline successfully continue breastfeeding without issues.
If you’re on medication and breastfeeding, you’re not alone. Thousands of mothers in the UK and beyond manage this every day. With the right information and timing, you can protect your baby’s health-and your own.
Henry Ward
December 30, 2025 AT 07:27This is the most irresponsible medical advice I've seen in years. You're telling mothers to just 'time' opioids around feeds like it's a coffee schedule? Hydrocodone is a Schedule II controlled substance with known neonatal depression risks. You're normalizing addiction in new moms while pretending it's all just pharmacokinetics. The AAFP doesn't approve of this-they warn against opioid use entirely in breastfeeding unless absolutely necessary. This isn't science, it's a dangerous loophole for lazy prescribers.
Aayush Khandelwal
December 31, 2025 AT 17:08Wow, this is like a pharmacokinetic symphony-beautifully orchestrated! The peak-trough dance between maternal plasma and breast milk is a masterpiece of biochemistry. When you factor in the RID (Relative Infant Dose) and the hepatic immaturity of neonates, you're essentially choreographing a molecular tango. I mean, who knew that a 3-hour half-life could be the difference between a serene infant and a sleepy little ghost? The LactMed app? That's not just a tool-it's a digital dharma wheel for the modern nursing yogi. 🙏
Sandeep Mishra
December 31, 2025 AT 18:43Hey everyone, I just wanted to say thank you for sharing this. As a dad who’s been through this with my wife, I know how overwhelming it feels. You’re not alone. I remember sitting up at 3am with a spreadsheet of half-lives and feeding times-it felt like rocket science. But honestly? The biggest help wasn’t the apps or the charts. It was finding a lactation consultant who didn’t judge us. If you’re stressed, reach out. There are people who get it. We’ve all been there. 💙
Joseph Corry
January 2, 2026 AT 08:31While the piece is superficially well-researched, it fundamentally misunderstands the epistemology of maternal pharmacology. The very premise of 'timing' assumes a Cartesian separation between mother and infant, when in reality, the lactating body is a bio-psycho-social continuum. The RID metric is a reductive quantification of an ontological entanglement. Moreover, the reliance on LactMed as a 'trusted' source is problematic-it's a database, not a phenomenological framework. Where is the hermeneutics of maternal suffering here? Where is the ethics of pharmaceutical normalization? This is not guidance-it's neoliberal medical management disguised as empowerment.
Colin L
January 2, 2026 AT 12:11Look, I get it, you're trying to be helpful, but you're glossing over the real issue: the medical system is failing mothers. My sister took sertraline for postpartum depression and her baby developed severe reflux and colic. She was told 'it's fine' because the RID was under 1%. But what about cumulative exposure? What about the fact that her baby’s liver was still developing? And then they told her to 'pump and dump'-as if that’s a solution and not a punishment. And don’t get me started on how the NHS barely has any lactation consultants left. You’re giving mothers a checklist while the system crumbles around them. This isn’t empowerment-it’s victim-blaming with citations.
Hayley Ash
January 3, 2026 AT 14:48kelly tracy
January 5, 2026 AT 07:21This article is a disaster. You’re telling women to 'time' their meds like they’re scheduling a Zoom call. What about the ones who can’t wait 4 hours between feeds because their baby is cluster feeding? What about the ones with low supply who can’t afford to pump and dump? You act like every mom has a freezer full of milk, a supportive partner, and a 9-to-5 job. I had a NICU baby. I was on hydrocodone after a C-section. I pumped every 3 hours. I cried every night. This isn’t 'balance'-it’s guilt wrapped in jargon. And now you want me to download an app? No. I want a system that doesn’t make me feel like a criminal for needing help.
srishti Jain
January 5, 2026 AT 10:18Cheyenne Sims
January 6, 2026 AT 11:25The use of the term 'pump and dump' is both grammatically incorrect and medically imprecise. The correct terminology is 'express and discard.' Furthermore, the reference to 'LactMed' without citing the National Library of Medicine's official publication ID or DOI is academically negligent. This article lacks proper attribution and employs colloquialisms that undermine its credibility. The American Academy of Pediatrics guidelines require formal documentation of drug exposure-this does not meet that standard.
Shae Chapman
January 7, 2026 AT 12:15OMG I LOVE THIS POST!!! 🥹💖 I was SO scared after my C-section and they gave me oxycodone-I followed this exact timing and my baby slept like an angel! I even set reminders on my phone with the LactMed app and it felt like I had a tiny medical team in my pocket 🤖💕 I cried when I saw how little transferred into my milk. You’re not alone, mama. You’re doing AMAZING. Keep going. You’re a superhero. 🦸♀️🍼✨
Nadia Spira
January 9, 2026 AT 10:36Let’s be real: this entire framework is a placebo for maternal anxiety. You’re giving women a false sense of control over an inherently uncontrollable biological process. The RID scale? A statistical illusion. Half-lives? Context-dependent variables in a system that varies by 40% between individuals. You’re not empowering mothers-you’re commodifying their fear into a checklist. And let’s not forget the irony: the same institutions pushing this 'safe timing' protocol are the ones that cut postpartum mental health services. This isn’t science. It’s capitalism with a stethoscope.
henry mateo
January 10, 2026 AT 16:43thanks for this i was so worried about my pain meds after my baby was born. i took ibuprofen after feeding and he was totally fine. i think i messed up once and took it right before and he was a little sleepy but not bad. i didnt know about lactmed but just downloaded it now. thanks again. you saved my sanity lol
Sandeep Mishra
January 12, 2026 AT 08:31Henry, I hear your concern-and you’re right that opioids carry risks. But the goal here isn’t to normalize them, it’s to minimize harm. For moms who need them after surgery or severe trauma, avoiding them entirely can lead to unmanaged pain, which increases stress hormones and actually reduces milk supply. Timing isn’t about convenience-it’s about harm reduction. We’re not saying ‘take anything anytime.’ We’re saying: ‘Here’s how to do it as safely as possible when you have no other option.’ And yes, alternatives matter. But sometimes, the alternative is suffering in silence. That’s not better.