How to Verify Dose Changes and Avoid Miscommunication in Healthcare

Getting a medication dose wrong can kill someone. It’s not a hypothetical. In 2022, over 1,200 reported incidents of incorrect dose changes led to nearly 300 patients being harmed. Most of these weren’t due to laziness or incompetence-they happened because systems failed, communication broke down, and verification became a checkbox instead of a safety net.
Why Dose Verification Isn’t Optional
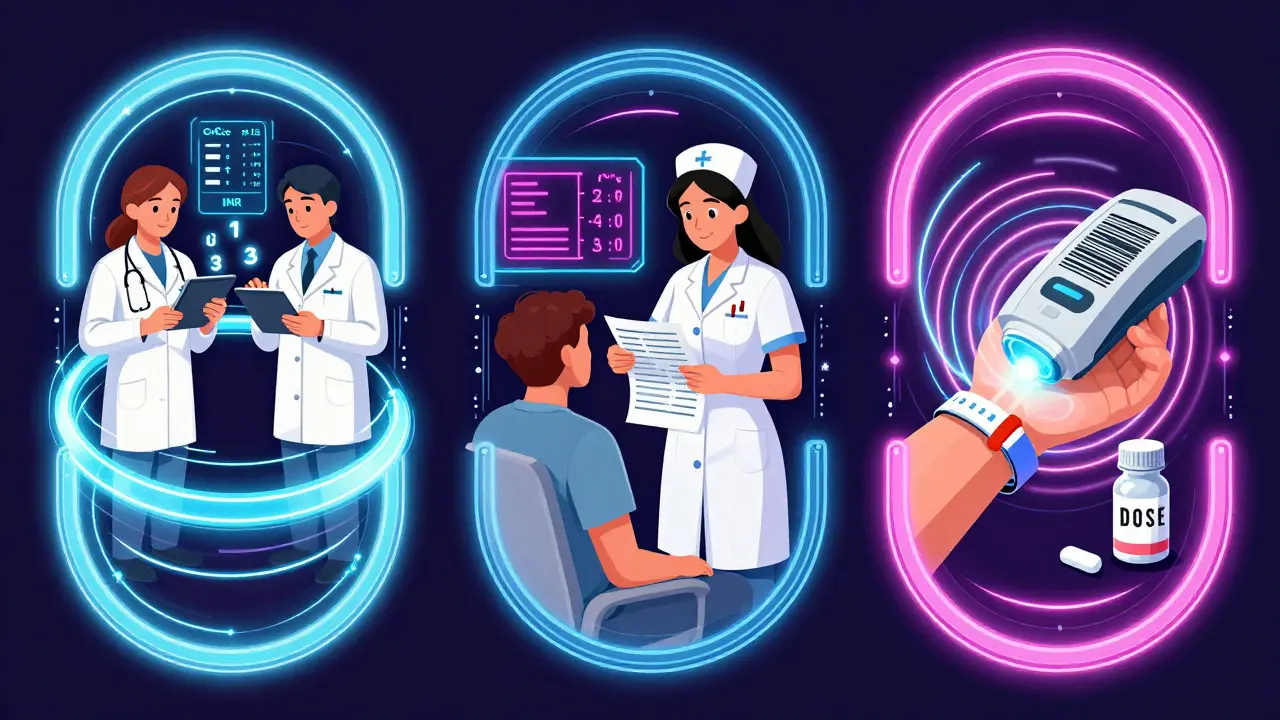
Medication errors are the third leading cause of death in U.S. hospitals. And the biggest risk? Dose changes. A simple typo-writing "10U" instead of "1.0U"-can mean ten times the insulin. A nurse rushing during shift change might miss a renal adjustment. A barcode scanner might not catch a wrong concentration if the system thinks it’s "correct" because the numbers look right. The Institute for Safe Medication Practices (ISMP) calls this the "perfect storm"-a mix of human fatigue, flawed tech, and unclear communication. But it doesn’t have to be this way. The fix isn’t more rules. It’s smarter verification.The 3-Step Verification Process That Works
Forget the old "double check everything" mantra. That’s exhausting, and it breeds complacency. The real solution? A targeted, three-step process backed by data:- Independent calculation-Two qualified staff members calculate the dose separately, without talking. For insulin, heparin, or opioids, this means recalculating based on weight, renal function, and lab values. Takes 2-3 minutes.
- Context cross-check-Verify the dose against the patient’s current condition. Is their creatinine clearance down? Did their INR spike? Did they just start a new drug that interacts? This step takes 1-2 minutes and stops errors before they reach the bedside.
- Barcode confirmation at the point of care-Scan the patient’s wristband, the drug, and the dose. This catches the wrong patient, wrong drug, or wrong vial. Takes 30-60 seconds.
When to Use Double Checks (and When Not To)
You’ve heard "always double check." But that’s dangerous advice. The Joint Commission found that 65% of medication error sentinel events trace back to miscommunication during dose changes-not lack of double checks. And overusing them makes people tune out. Use independent double checks only for high-alert medications:- Insulin (all forms)
- Heparin (especially IV)
- Opioids (morphine, fentanyl, hydromorphone)
- Chemotherapy agents
- Warfarin (due to narrow therapeutic index)
- IV potassium chloride
How Communication Breaks Down-And How to Fix It
The biggest threat isn’t the calculator. It’s the handoff. A nurse gets a new order at 7:15 a.m. The resident writes "increase fentanyl by 5 mcg/hr." The night nurse didn’t document the patient’s last pain score. The day nurse assumes it’s fine. Two hours later, the patient’s respirations slow. This happens because communication is sloppy. The fix? Use SBAR-Situation, Background, Assessment, Recommendation.- Situation: "Patient 42, post-op hip, on fentanyl PCA. Pain score increased from 3 to 7 in last hour."
- Background: "Fentanyl was increased from 10 to 15 mcg/hr yesterday. No recent labs. CrCl 62 mL/min."
- Assessment: "I believe the dose needs to go to 20 mcg/hr to control pain."
- Recommendation: "Can we order 20 mcg/hr and re-evaluate in 30 minutes?"
Technology Helps-But It’s Not a Magic Bullet
Barcode scanning prevents 86% of wrong-drug, wrong-patient, and wrong-dose errors. Smart infusion pumps with dose-error reduction software stop 85% of overdose attempts. But here’s the catch:- Barcode systems can’t detect a wrong concentration. A pharmacist enters 10 mg/mL instead of 1 mg/mL-but the system thinks it’s correct because the dose (1 mL) matches the order.
- Smart pumps don’t catch wrong-patient errors if the barcode is scanned on the wrong person.
- Alert fatigue is real. Nurses report ignoring 85% of BCMA alerts during busy shifts.
What Gets Measured Gets Improved
If you don’t document verification, it didn’t happen. Incomplete documentation caused 29% of verification failures in 2022, according to the Agency for Healthcare Research and Quality. Every verification must record:- Time of verification
- Names and credentials of both verifiers
- Confirmation of patient-specific factors (e.g., "CrCl 45 mL/min, weight 72 kg, INR 2.8")
- Final confirmation of barcode match

The Real Problem: Workload and Fatigue
Nurses aren’t ignoring protocols because they’re careless. They’re skipping them because they’re overwhelmed. A 2022 American Nurses Association survey found 73% of nurses admitted skipping verification steps during 12-hour shifts. Why? Nurse-to-patient ratios above 1:5 dropped verification adherence by 43%. Shift changes between 6-8 a.m. and p.m. accounted for 61% of verification failures. The answer isn’t to work harder. It’s to protect time. Johns Hopkins introduced "safety time"-15-20 minutes per shift where no other tasks are allowed. Just verification, communication, and documentation. Result? 22% fewer errors and 18% less nurse burnout.What’s Next: AI, Voice, and Blockchain
The future isn’t just better checks-it’s smarter systems.- AI tools like Epic’s DoseRange Advisor now flag abnormal dose changes before they’re even ordered-cutting inappropriate changes by 52% in a 12-hospital trial.
- Voice recognition systems let nurses say, "Verify insulin 5 units for patient Smith," and auto-log the check. Mayo Clinic pilots cut documentation time by 65%.
- Blockchain is being tested to create tamper-proof audit trails for every dose change, especially in transitions of care.
What You Can Do Today
You don’t need a $2 million system to make a difference. Start here:- Identify your top 5 high-alert medications. Apply the 3-step verification only to those.
- Train your team on SBAR. Practice it in huddles. Don’t just say it-use it.
- Block 15 minutes per shift for verification. Protect it like a code blue.
- Document every verification. No shortcuts. If it’s not written, it didn’t happen.
- Speak up when you see a dose that looks wrong-even if it’s from a doctor you respect.
What is the most common cause of dose verification failure?
The most common cause is miscommunication during shift changes, especially when critical details like renal function, recent lab values, or pain scores aren’t clearly passed on. Studies show 65% of medication error sentinel events involve breakdowns in handoff communication. The fix isn’t more checks-it’s structured communication like SBAR.
Do barcode scanners catch all dosing errors?
No. Barcode systems are excellent at catching the wrong patient, wrong drug, or wrong vial-but they can’t detect wrong concentration or wrong dose if the system thinks it’s correct. For example, if a drug is labeled as 10 mg/mL instead of 1 mg/mL, but the dose ordered is 1 mL, the scanner won’t flag it. Human verification is still essential for concentration and calculation errors.
Should every medication dose be double-checked?
No. The Institute for Safe Medication Practices advises against universal double checks because they create fatigue and false security. Focus them only on high-alert medications like insulin, heparin, opioids, chemotherapy, and warfarin. For other medications, a single verification with barcode scanning and clear documentation is sufficient and more sustainable.
How long should a dose verification take?
A proper 3-step verification takes 5-7 minutes total: 2-3 minutes for independent calculation, 1-2 minutes for patient context review, and 30-60 seconds for barcode confirmation. While this seems long, hospitals that protect this time see fewer errors and less burnout. Rushing it defeats the purpose.
What’s the biggest mistake in dose verification?
The biggest mistake is treating verification as a formality. When staff check boxes without thinking-like scanning a barcode while distracted or assuming a doctor’s order is correct without cross-checking-it becomes a ritual, not a safety net. Real verification requires active engagement, critical thinking, and a willingness to question-even when it’s uncomfortable.
Jennifer Littler
January 11, 2026 AT 13:20Just saw this at my hospital last week-nurse missed the renal adjustment on a heparin drip because she was rushing between 12 patients. We’ve started using the 3-step verification for high-alert meds only, and honestly? It’s the first time in years I’ve felt like the system actually protects us, not just checks boxes. The SBAR script saved my ass during a shift change yesterday. No more guessing. Just clarity.
Sam Davies
January 11, 2026 AT 17:16Oh wow, another ‘magic bullet’ post. Let me guess-Johns Hopkins did it, so we all must now waste 7 minutes per dose like we’re in a hospital-themed TED Talk? Newsflash: most places don’t have the staffing to do this. You’re not solving the problem-you’re just making tired nurses feel guilty for not doing the impossible.
Alfred Schmidt
January 12, 2026 AT 20:21THIS IS WHY PEOPLE DIE. I’ve seen it. A nurse scanned a vial, thought ‘it’s close enough,’ didn’t double-check the concentration-patient coded. And now some guy writes a 2000-word essay like this is a ‘best practice’ and not a goddamn emergency? The system is broken, and you’re all just rearranging deck chairs while the iceberg is still coming. Someone needs to get fired. And then someone else. And then the whole damn chain.
Priscilla Kraft
January 14, 2026 AT 06:38Thank you for writing this!! 🙏 I work in a small ER and we’ve been struggling with dose errors since the EMR upgrade. We started using SBAR in handoffs last month-and OMG-it’s changed everything. Even the docs are using it now. I cried when my coworker said ‘I’m not rushing this, I need 5 minutes.’ We’re not perfect, but we’re trying. You’re not alone. 💪❤️
Michael Patterson
January 15, 2026 AT 19:59Look, I’ve been in this game for 20 years, and I’ve seen every fad come and go-SBAR, barcode, double checks, AI, blockchain… none of it matters if the nurses are burnt out and the hospital is cutting staff to boost profits. You can have the perfect protocol, but if you’ve got one RN for 8 patients and 3 codes going on, you’re not gonna get perfect verification. You’re gonna get someone skipping steps because they’re afraid they’ll miss a cardiac arrest. The real problem? Management doesn’t care until someone dies. And even then, they just add another form.
Matthew Miller
January 16, 2026 AT 06:25So let me get this straight-you want us to add 7 minutes per high-alert med, but you won’t fix the staffing ratios that make it impossible? You want us to use SBAR, but you won’t train the damn residents who write ‘increase fentanyl by 5’ without context? This isn’t a solution-it’s a performance review checklist disguised as safety. You’re blaming the nurse for not doing the impossible while the hospital cuts hours and ignores the root cause: systemic neglect.
Adewumi Gbotemi
January 17, 2026 AT 05:17From Nigeria, I read this and thought-this is what we need back home. We don’t have barcode scanners or smart pumps. But we do have nurses who care. We use paper lists, shout across the ward, and check each other’s math. It’s messy. But it works. Maybe the real lesson is: even with nothing, if people talk and listen, lives are saved. Tech helps, but heart matters more.
Sean Feng
January 18, 2026 AT 16:35Yeah whatever. I scan the barcode. I check the dose. Done. If the system says it’s right, it’s right. I’m not a pharmacist. I’m not a math wizard. I’m just trying to get through my shift without getting yelled at. You want me to do 7 minutes of verification? Fine. But don’t blame me when the system crashes or the printer jams and I skip it. It’s not my fault.
Christian Basel
January 18, 2026 AT 23:01Let’s be real: the 3-step process is just a glorified audit trail. It doesn’t prevent errors-it just documents them after the fact. And who’s gonna audit the auditors? The real issue is that hospitals treat verification as a compliance task, not a clinical one. You’re training people to check boxes, not think. And that’s why mistakes keep happening. This is theater, not safety.
Alex Smith
January 19, 2026 AT 11:40So you’re telling me that a 22% drop in errors at Johns Hopkins is just because they added 15 minutes of ‘safety time’? That’s the whole secret? No fancy AI, no blockchain, no $500k software? Just… time? And respect? And people being allowed to pause? Huh. I guess the most advanced tech in healthcare isn’t tech at all. It’s just… not being a jerk about time.
Roshan Joy
January 20, 2026 AT 01:26Love this. I’m a nurse in India, and we don’t have all the tech you guys have. But we do have teamwork. We call out doses out loud, even if it’s just a simple acetaminophen. We say the name, the dose, the route. Sometimes the patient even repeats it. It’s old-school, but it works. And honestly? It builds trust. Not just in the system-but in each other. Keep it simple. Keep it human.
Madhav Malhotra
January 21, 2026 AT 20:33Man, this made me smile. We had a similar thing in our ward-nurses started using ‘safety time’ and now we all take a breath before we give meds. Even the interns join in. We don’t call it SBAR-we call it ‘the pause.’ It’s not perfect, but now when someone says ‘hold on, let me check,’ no one rolls their eyes. We actually mean it. That’s the win.
Priya Patel
January 23, 2026 AT 03:48Okay I just had to comment-this is the most hope I’ve felt in my nursing career. 😭 I’ve been on the edge of quitting because I felt like I was just a cog in a broken machine. But reading this? It’s like someone finally said: ‘Your brain matters. Your voice matters. Your pause matters.’ I’m going to start SBAR tomorrow. And I’m gonna block my 15 minutes. No excuses. 💙