Hypertensive Retinopathy: How High Blood Pressure Damages Your Eyes

When your blood pressure stays too high for too long, it doesn’t just strain your heart and arteries-it quietly starts wrecking the tiny blood vessels in your eyes. This isn’t just a theory. It’s happening right now in millions of people who think their vision is fine because they haven’t noticed any changes. But by the time they do, it might be too late to fully reverse the damage. This is hypertensive retinopathy, and it’s one of the most silent but serious consequences of uncontrolled high blood pressure.
What Exactly Is Hypertensive Retinopathy?
Hypertensive retinopathy is damage to the retina-the light-sensitive layer at the back of your eye-caused by long-term high blood pressure. The retina relies on a network of tiny, delicate blood vessels to deliver oxygen and nutrients. When blood pressure stays elevated, these vessels get squeezed, thickened, and sometimes blocked. Over time, they leak fluid or blood, starve parts of the retina, and trigger swelling. The result? Vision changes that start subtle and can end in permanent blindness.
This isn’t something that happens overnight. It takes years. But once it starts, it doesn’t stop unless you act. Studies show that even people with "mild" hypertension-systolic pressure between 130 and 139 mmHg-can develop retinal damage after 10 years without treatment. And if your pressure is consistently above 160/100 mmHg? The risk jumps dramatically.
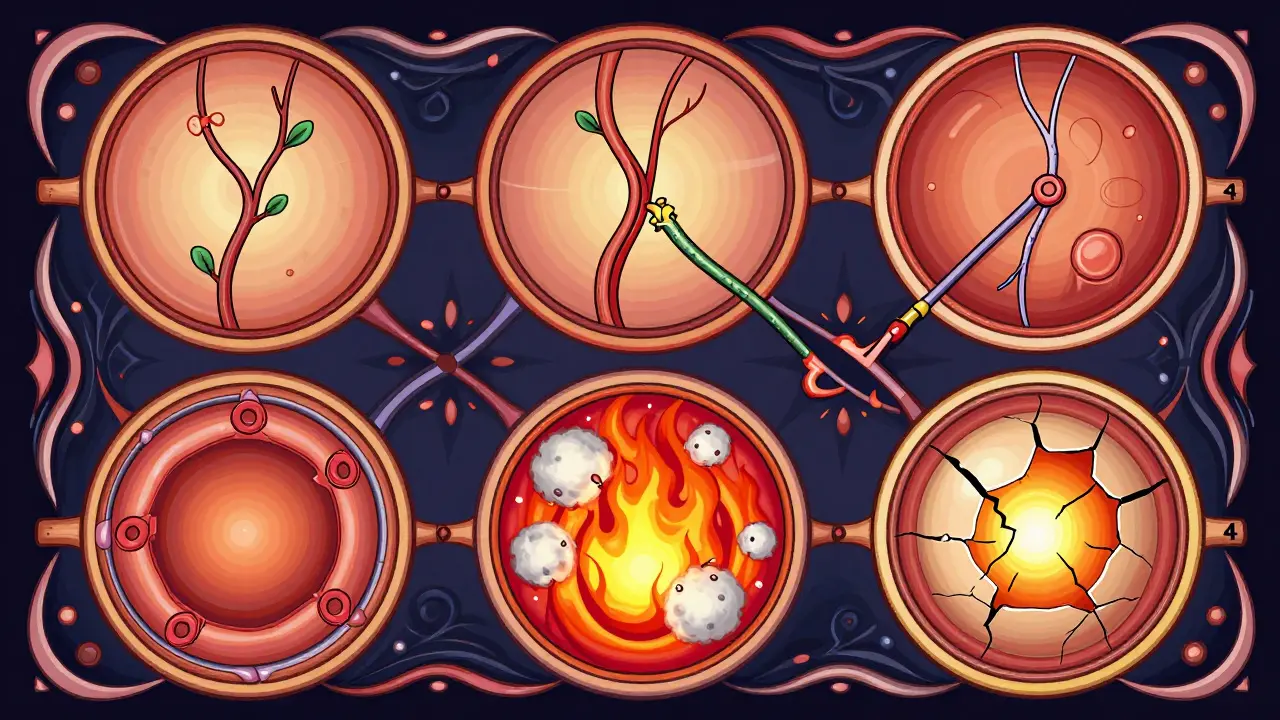
The Four Stages of Retinal Damage
Doctors classify hypertensive retinopathy into four clear stages using the Keith-Wagener-Barker system. It’s not just a label-it’s a roadmap of how bad things have gotten.
- Grade 1: The earliest sign. Blood vessels in the retina start to narrow slightly-by about 15 to 25%. You won’t notice anything. No blurriness. No spots. Just a subtle change visible only on a professional eye exam.
- Grade 2: The narrowing gets worse. Now, you see "arteriovenous nicking"-where an artery presses down on a vein like a thumb on a garden hose. This disrupts blood flow. Still, most people have no symptoms. But this stage means your blood pressure has been high for at least 3 to 5 years.
- Grade 3: Now things get serious. You start seeing retinal hemorrhages (tiny bursts of bleeding), cotton wool spots (areas where nerve fibers are starving from lack of blood), and hard exudates (yellowish lipid deposits). This is when vision starts to blur. About 85% of people at this stage report vision problems. And if you’re here, your risk of stroke or heart attack is 2.5 times higher than someone with normal blood pressure.
- Grade 4: This is a medical emergency. Swelling of the optic disc (papilledema) appears. It means pressure is so high that fluid is leaking into the brain’s protective lining. People often describe sudden "curtain-like" vision loss or double vision. At this point, 78% of patients have already suffered damage to their kidneys or heart. And if diastolic pressure hits 120 mmHg or higher? About 40% develop optic disc swelling within 72 hours.
Why You Might Not Notice It Until It’s Too Late
Here’s the scary part: 68% of people with early-stage hypertensive retinopathy (Grades 1 and 2) feel perfectly fine. No headaches. No blurred vision. No warning signs. That’s why so many wait until they’re in Grade 3 or 4 before seeing a doctor.
One Reddit user, u/RetinaWarrior, described waking up with dark spots in the center of their vision after their blood pressure spiked to 210/110. Another mentioned double vision and severe headaches-symptoms they ignored for months, thinking it was stress. By the time they went to an ophthalmologist, they’d already lost part of their peripheral vision.
Clinical data shows that 42% of patients delay seeking help until their daily life is disrupted-reading the newspaper, driving at night, or recognizing faces becomes hard. The average time between first symptoms and diagnosis? 18 to 24 months. That’s a lot of damage in just over a year.
How Doctors Spot It
A routine eye exam with a fundoscope can catch early signs. But technology is making it even better. Optical coherence tomography (OCT) now shows retinal thickness changes as small as 10%-a sign of fluid buildup before you can see it. AI tools like IDx-DR and the FDA-approved RetinaCheck AI are now helping doctors detect patterns in retinal images with 92% accuracy, up from 75% just a few years ago.
What they’re looking for:
- Arteriovenous nicking
- Flame-shaped hemorrhages (500-1000 microns wide)
- Hard exudates (lipid deposits around leaking vessels)
- Cotton wool spots (tiny white patches from nerve fiber damage)
- Optic disc swelling (Grade 4)
These aren’t random findings. They’re direct indicators of how hard your blood pressure is pounding on your entire vascular system. In fact, the condition is called a "window to systemic vascular health"-because if your eye vessels are damaged, so are your heart, kidneys, and brain.
What Happens If You Ignore It
Untreated hypertensive retinopathy doesn’t just hurt your vision. It’s a warning sign that you’re at high risk for:
- Stroke (3.2x higher risk if you have AV nicking or papilledema)
- Heart attack
- Chronic kidney disease
- Heart failure
And here’s the kicker: once the macula (the center of your vision) is damaged by lipid deposits or bleeding, recovery is slow-or impossible. Even with perfect blood pressure control, 22% of patients with severe retinopathy end up with permanent blind spots.
Diabetics are even more at risk. If you have both diabetes and high blood pressure, your chance of permanent vision loss is 4.7 times higher than someone with just one condition. The damage compounds.
Can You Reverse the Damage?
Yes-but only if you act fast.
Studies show that lowering systolic blood pressure by 25 mmHg within 24 to 48 hours can reverse early retinal changes in 65% of cases. That means if your pressure is 180/110, getting it down to 155/85 quickly can save your vision.
But speed matters. If you’re in Grade 4, with optic disc swelling, you need emergency treatment. Delaying even a few days can mean permanent damage.
Recovery isn’t instant. Vision improvement usually starts within 7 to 10 days of stabilizing blood pressure. Full healing can take 3 to 6 months. But if the retina has scarred or the optic nerve is dead? That’s irreversible.
What You Can Do
Here’s what works, based on real-world data:
- Check your BP regularly. Home monitors are cheap and accurate. Take readings twice a day for two weeks. If you’re over 40, or have any risk factors, do it yearly-even if you feel fine.
- Get your eyes checked. The American Academy of Ophthalmology says everyone with hypertension should have a dilated eye exam at least once a year. If your pressure is above 140/90 despite medication, do it every 6 months.
- Treat the root cause. ACE inhibitors (like lisinopril) reduce retinal damage progression by 32% more than calcium channel blockers, according to the European Society of Cardiology. Talk to your doctor about the best drug for your case.
- Use your meds. Only 15% of people link their vision problems to high blood pressure without a doctor’s warning. But if you stick to your treatment plan and get regular eye exams? Your odds of avoiding vision loss jump by 35%.
- Watch for red flags. Sudden blurred vision, dark spots, double vision, or a "curtain" coming down over your sight? Don’t wait. Go to the ER. Your eyes are telling you your body is in crisis.
The Bigger Picture
Hypertensive retinopathy isn’t just an eye problem. It’s a red flag that your whole body is under siege. Every leaky vessel in your retina is a sign that similar damage is happening in your brain, heart, and kidneys.
And the good news? You’re not powerless. The National Eye Institute found that with proper blood pressure control, 85% of early-stage cases stop progressing. That’s not a guarantee-but it’s a strong chance, if you act now.
Don’t wait for symptoms. Don’t assume "no symptoms = no problem." Your eyes are the only place in your body where doctors can see your blood vessels directly. Use that to your advantage.
Can hypertensive retinopathy cause blindness?
Yes, if left untreated. Advanced stages-especially Grade 4 with optic nerve swelling and macular damage-can lead to permanent vision loss. About 22% of patients with severe retinopathy develop irreversible blind spots even after blood pressure is controlled. Early detection and treatment are critical to prevent this.
How long does it take for high blood pressure to damage the eyes?
Damage can begin in as little as 3 to 5 years with uncontrolled hypertension. Even "mild" high blood pressure (130-139 systolic) can cause retinal changes after 10 years without treatment. The longer your pressure stays high, the worse the damage becomes. There’s no safe window-early intervention is key.
Do you need to see an eye doctor if you have high blood pressure?
Yes. The American Academy of Ophthalmology recommends a dilated eye exam at least once a year for anyone diagnosed with hypertension. If your blood pressure is above 140/90 mmHg despite medication, get checked every 6 months. Many people don’t realize eye exams can detect life-threatening risks long before symptoms appear.
Can lowering blood pressure improve vision in hypertensive retinopathy?
Yes-if caught early. Reducing systolic blood pressure by 25 mmHg within 24 to 48 hours reverses retinal changes in 65% of cases. Vision improvement usually starts within 7 to 10 days. However, if the macula or optic nerve is already scarred, full recovery isn’t possible. Speed and consistency in lowering BP make all the difference.
Is hypertensive retinopathy more dangerous for diabetics?
Extremely so. People with both diabetes and high blood pressure have a 4.7 times higher risk of permanent vision loss than those with only one condition. The damage from diabetic retinopathy and hypertensive retinopathy overlaps and accelerates. Tight control of both blood pressure and blood sugar is essential to protect vision.
What’s Next?
Research is moving fast. The NIH’s RETINA-HTN study is now testing genetic markers to identify who’s most at risk. New devices like RetiFlow are being tested to measure retinal blood flow without invasive dye injections. And AI is making screening faster and more accurate-even in primary care clinics.
But none of that matters if you don’t act. Your eyes are giving you signals. Listen to them. Check your blood pressure. Get your eyes checked. Take your meds. Don’t wait for the curtain to fall.