Hypocalcemia and Alcoholism: How Alcohol Triggers Low Calcium Levels

Hypocalcemia Risk Checker
Check Your Symptoms
Select all symptoms you experience:
Alcohol Consumption
Imagine enjoying a night out, feeling the buzz, while inside your body a silent shortage of calcium is building up. That hidden imbalance is called hypocalcemia, and heavy drinking is one of the sneakiest culprits.
What Is Hypocalcemia?
Hypocalcemia is a medical condition where the concentration of calcium in the blood falls below the normal range (usually under 8.5 mg/dL). Calcium is the body’s main mineral for bone strength, muscle contraction, nerve signaling, and blood clotting, so a drop can affect many systems.
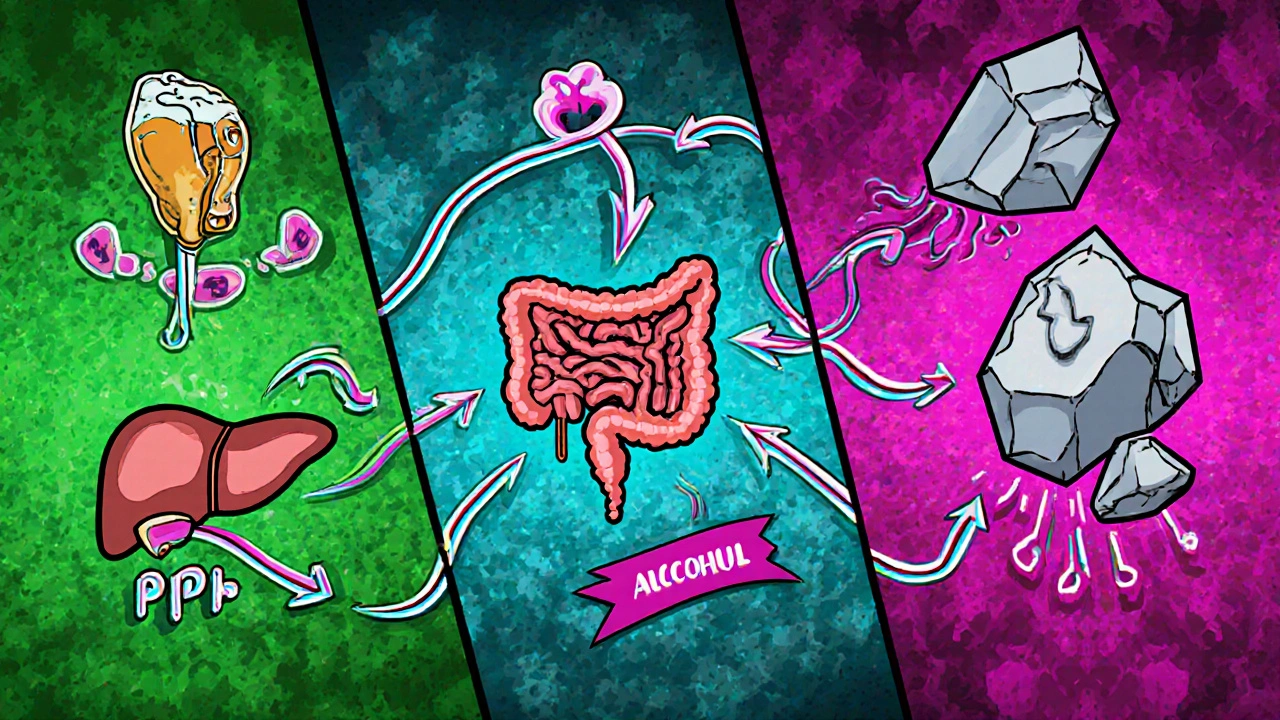
How Alcohol Affects Calcium Levels
Alcoholism refers to a chronic pattern of drinking that leads to physical or mental health problems. When alcohol enters the bloodstream, it interferes with several processes that keep calcium balanced.
- Parathyroid hormone suppression: Alcohol can blunt the release of Parathyroid hormone (PTH), the hormone that tells bones, kidneys, and intestines to release or retain calcium.
- Vitamin D activation gets hit hard. The liver, which converts Vitamin D into its active form, often suffers damage in heavy drinkers. Less active Vitamin D means the gut absorbs less calcium.
- Magnesium depletion is common with alcohol abuse. Low magnesium impairs PTH secretion and its action, creating a double‑whammy on calcium.
- Chronic liver disease itself disrupts protein synthesis, affecting the proteins that bind calcium in the blood.
All these pathways funnel into the same outcome: the body can’t keep calcium where it belongs, leading to hypocalcemia.
Typical Symptoms When Alcohol Meets Low Calcium
Because calcium touches nerves and muscles, people often notice these signs:
- Muscle cramps or tingling, especially around the mouth and fingers (often called "perioral paresthesia").
- Sudden muscle spasms or "tetany" - uncontrollable jerks that can feel frightening.
- Heart palpitations or an irregular heartbeat, since calcium helps the heart contract.
- Bone pain or increased fracture risk over time, linked to Bone health deterioration.
- Severe cases may lead to seizures or confusion.
Many of these symptoms overlap with other alcohol‑related issues, which is why the problem often stays undetected.
Diagnosing the Problem: Tests Doctors Use
When a clinician suspects hypocalcemia, they order a handful of straightforward labs:
- Serum calcium test - measures total calcium in the blood.
- Ionized calcium - the active form that truly reflects physiological status.
- Parathyroid hormone (PTH) level - helps separate PTH‑related causes from others.
- 25‑hydroxy Vitamin D - checks whether a deficiency is feeding the problem.
- Magnesium and phosphate - low values often accompany alcohol‑induced hypocalcemia.
- Liver function panel - identifies chronic liver disease that may be at play.
The results paint a clear picture: low calcium paired with low or inappropriately normal PTH points strongly toward alcohol‑related suppression.
Managing and Treating Alcohol‑Related Hypocalcemia
Treatment starts with two priorities: raise calcium back to safe levels and address the alcohol factor.
- Acute correction: In severe cases, doctors give intravenous calcium gluconate to quickly normalize blood levels.
- Oral supplementation: Calcium carbonate or calcium citrate tablets, often combined with Vitamin D (e.g., cholecalciferol), support steady recovery.
- Magnesium repletion: Since magnesium is a co‑factor, oral magnesium oxide or citrate can boost PTH effectiveness.
- Address liver health: Reducing alcohol intake, using liver‑supportive nutrients, and, when needed, consulting a hepatologist can restore Vitamin D activation.
- Long‑term alcohol counseling: Referral to addiction services, counseling, or medication‑assisted therapy (e.g., naltrexone) helps prevent recurrence.
Regular follow‑up labs every 4‑6 weeks ensure calcium stays in range and that the underlying causes are being managed.

Prevention Tips for Drinkers
If you enjoy a drink but want to keep calcium in check, try these simple habits:
- Limit intake to moderate levels - up to one drink per day for women, two for men.
- Include calcium‑rich foods daily: dairy, fortified plant milks, leafy greens, or tofu.
- Boost Vitamin D with safe sun exposure or a daily supplement (800‑1,000 IU).
- Stay on top of magnesium - nuts, seeds, whole grains, and legumes are good sources.
- Schedule annual blood work if you have a history of heavy drinking; early detection stops problems before they flare.
Quick Checklist for Health Professionals
| Cause | Mechanism | Typical Lab Pattern |
|---|---|---|
| Alcoholism | PTH suppression, Vitamin D activation loss, Mg deficiency | Low Ca, low/normal PTH, low Mg, low 25‑OH Vitamin D |
| Hypoparathyroidism | Insufficient PTH production | Low Ca, low PTH, normal Mg, normal Vitamin D |
| Vitamin D deficiency | Reduced intestinal Ca absorption | Low Ca, high PTH, low 25‑OH Vitamin D |
| Acute pancreatitis | S‑protein binds calcium, fat saponification | Low Ca, variable PTH, elevated lipase |
Frequently Asked Questions
Can occasional binge drinking cause hypocalcemia?
A single binge episode may lower calcium slightly, but clinically significant hypocalcemia usually appears after repeated heavy drinking that damages the liver or depletes magnesium.
What’s the difference between total calcium and ionized calcium?
Total calcium measures calcium bound to proteins plus the free portion. Ionized calcium is the biologically active form. In some alcohol‑related cases, protein levels shift, so ionized calcium gives a more accurate picture.
Will calcium supplements alone fix the problem?
Supplements help, but without correcting vitamin D, magnesium, and the underlying alcohol use, calcium levels often bounce back down. A combined approach works best.
Is hypocalcemia reversible?
Yes. When alcohol consumption is reduced or stopped and the missing nutrients are replenished, calcium levels typically return to normal within weeks to months.
Should I get screened for bone loss if I’ve had low calcium?
A bone density scan (DEXA) is advisable if you’ve had chronic hypocalcemia, especially with a history of heavy drinking, because low calcium can erode bone over time.
Demetri Huyler
October 20, 2025 AT 22:28Alcoholics are just killing their bones, plain and simple.
JessicaAnn Sutton
October 20, 2025 AT 23:26Chronic ethanol consumption undeniably suppresses parathyroid hormone release, which in turn impairs calcium homeostasis.
The cascade of vitamin D activation loss and magnesium depletion further compounds the deficit.
Consequently, patients present with tetany, paresthesia, and potential cardiac arrhythmias.
Addressing these metabolic derangements requires both supplementation and cessation of alcohol.
Israel Emory
October 21, 2025 AT 00:40Listen up, the link between booze and calcium isn’t some mystical rumor, it’s solid biochemistry.
Ethanol messes with the parathyroid glands, throttling PTH secretion right when your body needs it most.
Without enough PTH, your bones stop releasing calcium and your kidneys reabsorb less of it.
At the same time, the liver-already taking a beating from chronic drinking-fails to convert vitamin D to its active form.
Inactive vitamin D means the gut can’t pull in the calcium you eat, leaving the bloodstream starved.
Don’t forget magnesium; alcohol depletes it, and low magnesium further blunts PTH’s effectiveness, creating a perfect storm.
The clinical picture shows up as muscle cramps, perioral tingling, even seizures if you push it far enough.
Cardiac muscle isn’t immune either; low calcium can precipitate arrhythmias that are life‑threatening.
What’s more, chronic hypocalcemia erodes bone density over time, setting the stage for fractures later in life.
You can run the standard labs-serum calcium, ionized calcium, PTH, 25‑OH vitamin D, magnesium-to confirm the diagnosis.
If the labs show low calcium with low or inappropriately normal PTH, you’ve got the classic alcohol‑induced pattern.
Treatment isn’t just about slapping on calcium tablets; you need to replenish magnesium and boost vitamin D concurrently.
Intravenous calcium gluconate can save a patient in acute tetany, but the real fix is to quit the alcohol and repair liver function.
Long‑term follow‑up every month or two ensures the numbers stay in range and that you’re not slipping back into old habits.
Bottom line: ignore the booze, and your calcium system will bounce back, but keep the bottles at bay and you’ll avoid the whole cascade.
Sebastian Green
October 21, 2025 AT 01:30I’ve seen friends go through this, and the fear of seizures is real; getting proper labs early can make all the difference.
Alex Pegg
October 21, 2025 AT 02:20Most people blame the liver, but the real issue is the ignored magnesium deficiency.
laura wood
October 21, 2025 AT 03:10Magnesium often flies under the radar, yet it’s essential for PTH action and overall calcium balance, so a balanced diet is key.
Kate McKay
October 21, 2025 AT 04:00If you’re cutting back on alcohol, start by adding calcium‑rich foods like dairy, fortified plant milks, and leafy greens.
Pair that with a daily vitamin D supplement around 800‑1000 IU to boost absorption.
Don’t overlook magnesium sources-nuts, seeds, and whole grains can keep your PTH humming.
Schedule a blood panel every few months; early detection of low calcium can prevent the nasty symptoms.
Stick to the plan, stay consistent, and you’ll see your levels stabilize.
Wesley Humble
October 21, 2025 AT 04:50While your recommendations are well‑intentioned, the literature indicates that calcium supplementation absent vitamin D correction yields only transient improvements 😊.
Moreover, randomized controlled trials demonstrate superior outcomes when magnesium repletion accompanies calcium therapy 📊.
Therefore, a comprehensive protocol is indispensable.
barnabas jacob
October 21, 2025 AT 05:40Yo, if u keep chuggin’ the hooch u’re basically invitin’ hypocalcemia to party in ur veins, lol.