Lyme Disease: Tick-Borne Infection and Treatment Timeline

When you get bitten by a tick, most people assume it’s no big deal. But in parts of the U.S. and Europe, a single bite can lead to something far more serious: Lyme disease. It’s not just a rash or a flu bug-it’s a bacterial infection that can spread through your body if not caught early. And the clock starts ticking the moment that tiny tick latches on.
How Lyme Disease Starts
Lyme disease is caused by a spiral-shaped bacterium called Borrelia burgdorferi. It’s carried by blacklegged ticks-small, dark, and easy to miss. These ticks don’t jump or fly. They wait on grass, bushes, or leaf litter, and grab onto you as you brush past. Nymph ticks, the size of a poppy seed, are the worst offenders. They’re active in spring and summer, when people are outdoors more, and they’re hard to spot until they’re already feeding.
Here’s the key fact: transmission doesn’t happen instantly. Research shows the bacteria need time to move from the tick’s gut to its saliva. Most sources agree it takes at least 24 hours, and sometimes up to 36, before the infection can spread. That’s why checking yourself after being outside matters so much. If you remove the tick within a day, your risk drops by 95%.
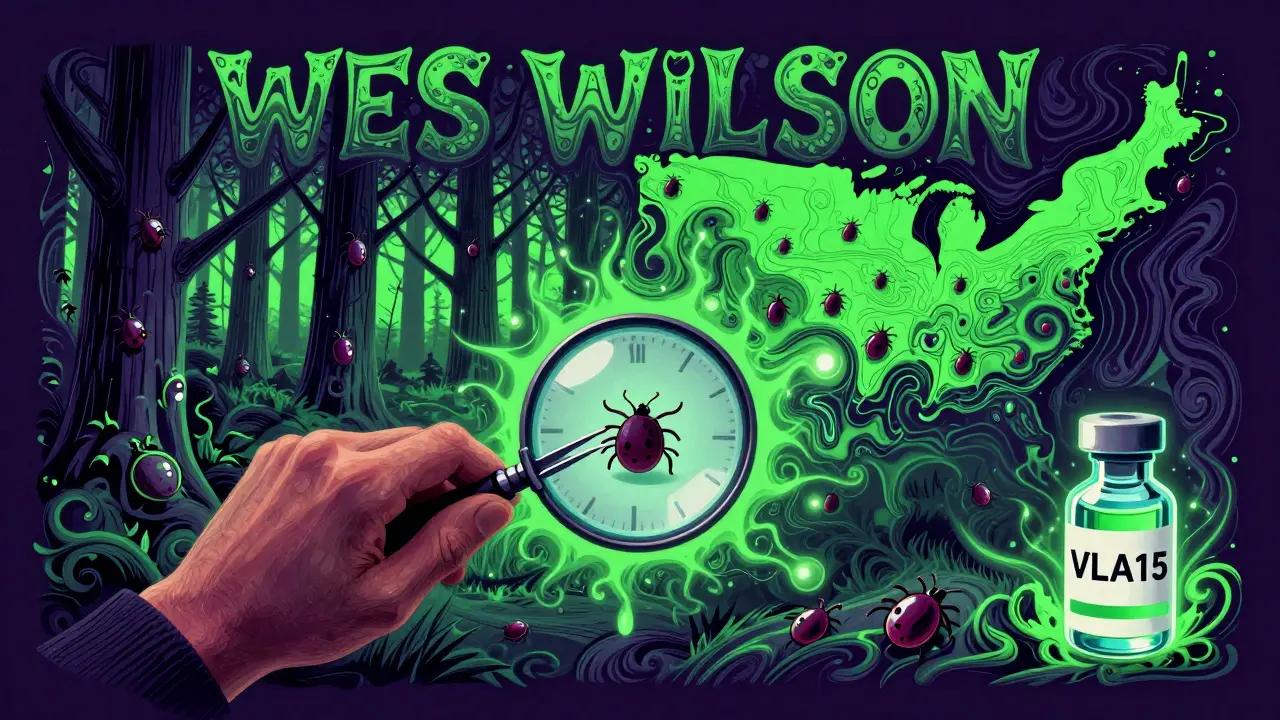
In the U.S., Lyme is most common in 14 states: Connecticut, New York, Pennsylvania, Wisconsin, and others in the Northeast and Upper Midwest. But climate change is shifting things. Ticks are moving north. Canada has seen a 50% expansion of tick habitat since 2000. That means more people in places like Ontario and Quebec are now at risk.
The Three Stages of Lyme Disease
Lyme doesn’t hit all at once. It unfolds in stages, each with clearer signs than the last.
Stage 1: Early Localized (1-28 days after bite)
This is when you’re most likely to notice something’s wrong. About 70-80% of people develop a rash called erythema migrans. It starts as a red spot, then expands outward, sometimes forming a bull’s-eye pattern. But not everyone gets the classic ring. Some see a solid red patch. Others don’t see any rash at all.
Alongside the rash, flu-like symptoms often show up: fever (in 45% of cases), chills, fatigue (70%), headaches (61%), and muscle aches. These are easy to blame on a cold or the flu-especially if you didn’t notice the tick. That’s why so many people delay diagnosis.
Stage 2: Early Disseminated (weeks to months)
If untreated, the bacteria spread. Now you’re not just dealing with a rash. You might get multiple rashes in different places. Neurological symptoms can appear: facial drooping (Bell’s palsy), numbness, or shooting pain. Heart problems like Lyme carditis can cause dizziness, shortness of breath, or an irregular heartbeat. About 4-10% of untreated cases develop this.
One patient I read about-a 32-year-old hiker from Vermont-started with knee pain. Two months later, he couldn’t lift his eyelid. He’d been misdiagnosed with arthritis. By the time he got the right test, the infection had reached his nervous system.
Stage 3: Late Disseminated (months to years)
This is what happens when Lyme is ignored for too long. About 60% of untreated patients develop severe joint pain, especially in the knees. It comes and goes, sometimes for years. Nerve damage can cause tingling, burning, or memory issues. Some people describe it as brain fog-trouble finding words, forgetting appointments, feeling exhausted even after sleep.
These aren’t rare. A 2021 survey by the Bay Area Lyme Foundation found 42% of patients still had symptoms six months after treatment. The biggest complaints? Fatigue (78%), cognitive trouble (65%), and joint pain (61%).

Treatment: What Works, What Doesn’t
Here’s the good news: if caught early, Lyme is almost always curable.
For Stage 1, doctors prescribe 10-21 days of oral antibiotics. Doxycycline is standard for adults. Kids and pregnant people get amoxicillin or cefuroxime. Most people feel better within days. Symptoms disappear in weeks. The CDC says 87% of patients treated within 30 days of symptoms fully recover within three months.
Stage 2 or 3? That’s where things get harder. You need intravenous antibiotics-usually ceftriaxone-for 14-28 days. Hospital visits. IV lines. Longer recovery. But even then, many people bounce back.
There’s controversy around what happens after treatment. Some patients still feel awful. That’s called Post-Treatment Lyme Disease Syndrome (PTLDS). It’s not an active infection. The bacteria are gone. But the body’s immune system might still be overreacting. About 10-20% of patients experience this. Johns Hopkins research shows it’s real, but it’s not the same as “chronic Lyme disease.”
Here’s where things get messy. Some clinics push long-term antibiotics for persistent symptoms. But the Infectious Diseases Society of America (IDSA) says there’s no proof that lingering bacteria cause these symptoms. And long-term antibiotics? They can cause serious side effects-C. diff infections, liver damage, antibiotic resistance.
Meanwhile, 28 U.S. states have passed laws protecting doctors who give long-term antibiotics for “chronic Lyme.” That’s not because science supports it. It’s because patients are desperate. And doctors are caught between evidence and empathy.
Testing: Why It’s Flawed
Doctors don’t just guess. They test. But the tests aren’t perfect.
The standard two-step blood test (ELISA then Western blot) only catches about 30% of cases in the first week. Why? Your body hasn’t made enough antibodies yet. It takes weeks. That’s why if you have the bull’s-eye rash, you don’t need a test. The rash alone is proof.
But what if you don’t have the rash? Then you’re stuck waiting. Or getting false negatives. A 2023 study in Emerging Infectious Diseases found current blood tests miss 35% of early Lyme cases.
That’s why the new MiQLick test, approved by the FDA in March 2023, matters. It detects bacterial DNA in urine-not antibodies. It’s 92% accurate in early disease. It’s not everywhere yet, but it’s a step toward faster, more reliable diagnosis.
Prevention: What You Can Actually Do
You can’t avoid ticks entirely. But you can cut your risk dramatically.
- Check your body within 2 hours of being outdoors-especially underarms, groin, scalp, and behind the knees.
- Shower soon after coming inside. It washes off unattached ticks.
- Use permethrin on clothes. It kills ticks on contact.
- Wear long pants tucked into socks in tall grass or wooded areas.
- If you find a tick, remove it with fine-tipped tweezers. Grasp close to the skin. Pull straight up. Don’t twist. Don’t crush it.
For high-risk areas, if the tick is engorged and attached for more than 36 hours, a single 200mg dose of doxycycline within 72 hours can prevent infection. It’s not for everyone-but if you’re in a hot zone, ask your doctor.
What’s Next?
Hope is growing. A new Lyme vaccine, VLA15, is in Phase 3 trials. It targets multiple strains of Borrelia and showed 70-96% effectiveness in early studies. If approved, it could be available by 2027.
Researchers are also testing mRNA vaccines-like the ones used for COVID-19. Early animal studies look promising. The National Institute of Allergy and Infectious Diseases plans human trials in 2024.
But until then, the best defense is awareness. Know the signs. Act fast. Don’t wait for a rash. Don’t assume it’s just a cold. If you’ve been in tick country and feel off for more than a few days, get checked.
Lyme disease isn’t a death sentence. But it’s a silent threat. And timing is everything.
Can you get Lyme disease from a dog or cat?
No, you can’t catch Lyme disease directly from pets. But dogs and cats can carry infected ticks into your home. If your pet has ticks, check yourself and your surroundings. Tick removal is just as important for pets. Use vet-approved preventatives like topical treatments or collars.
Is Lyme disease contagious between people?
No. Lyme disease cannot spread through touch, kissing, blood transfusions, or sexual contact. The only known transmission route is through the bite of an infected tick. Pregnant women with untreated Lyme can pass the infection to their unborn child, but proper antibiotic treatment prevents this.
Why do some people test negative even if they have Lyme?
Standard blood tests look for antibodies, which take weeks to develop. In the first few days after a bite, your body hasn’t made enough to show up on the test. That’s why the rash is the gold standard for diagnosis early on. If you have symptoms and live in a high-risk area, doctors should treat based on clinical signs-not just test results.
Can you get Lyme disease more than once?
Yes. Getting Lyme once doesn’t make you immune. You can be bitten again by another infected tick. That’s why ongoing prevention is critical-even if you’ve had it before. There’s no lasting protection from natural infection.
What’s the difference between Lyme disease and chronic Lyme disease?
Lyme disease is a confirmed bacterial infection with clear stages and treatment guidelines. "Chronic Lyme disease" isn’t a medically recognized diagnosis. It’s a term used by some patients and providers to describe lingering symptoms after treatment. The scientific consensus is that those symptoms are likely due to an overactive immune response (PTLDS), not ongoing infection. Long-term antibiotics aren’t proven to help and can cause harm.
Jacob den Hollander
February 7, 2026 AT 19:14Man, I just got back from a hike in Vermont, and now I’m paranoid. I didn’t even notice a tick, but my leg’s been itchy for two days. I checked the CDC map-yep, I was right in the hot zone. I’m gonna call my doc tomorrow and ask about that single-dose doxycycline thing. Better safe than sorry, right? I’ve read too many stories of people ignoring it and ending up with joint pain that won’t quit. I’m not gonna be one of them.
Also, I’m gonna start tucking my pants into my socks. Sounds ridiculous, but if it saves me from six months of brain fog, I’ll look like a hiker from 1998.
Andrew Jackson
February 7, 2026 AT 21:59It is a matter of profound national concern that the American public has grown so complacent regarding the encroachment of vector-borne disease upon our domestic ecosystems. The expansion of tick habitats into Canadian provinces is not merely an ecological shift-it is a symptom of systemic environmental negligence. We have allowed lax border controls, unregulated land development, and climate apathy to erode the very foundations of public health. This is not a medical issue. It is a failure of civic responsibility. The solution is not more antibiotics-it is a return to discipline, preparedness, and national vigilance.