Miglitol (Glyset) vs Alternative Diabetes Drugs - Complete Comparison
Diabetes Drug Selector Tool
Find Your Ideal Diabetes Medication
Answer a few questions to identify which oral diabetes medication might work best for your specific situation.
Trying to figure out whether Glyset (Miglitol) is the right choice for your type‑2 diabetes can feel like navigating a maze of drug names, doses, and side‑effects. This guide breaks down Miglitol and pits it against the most common oral alternatives, so you can see the strengths, weaknesses, and ideal patient profiles in plain English.
- Understand Miglitol’s mechanism and typical dosing.
- See a side‑by‑side comparison of efficacy, safety, and cost.
- Learn which patients benefit most from each option.
- Get practical tips for handling common side‑effects.
What is Miglitol (Glyset)?
Miglitol is a prescription oral medication classified as an alpha‑glucosidase inhibitor. It slows the breakdown of complex carbohydrates in the intestine, which reduces post‑meal blood‑glucose spikes. In the United States, it is marketed under the brand name Glyset and is approved for adults with type‑2 diabetes who need better post‑prandial glucose control.
How Miglitol Works and Typical Dosage
The drug targets the enzyme alpha‑glucosidase located on the brush border of the small intestine. By inhibiting this enzyme, Miglitol delays carbohydrate digestion, allowing glucose to enter the bloodstream more gradually. Most clinicians start patients on 25mg taken with the first bite of each main meal, titrating up to 100mg three times daily if needed. Because it works locally in the gut, it has minimal systemic absorption, which reduces the risk of drug‑drug interactions.
Key Criteria for Comparing Oral Diabetes Medications
When you line up Miglitol against other options, consider these five factors:
- Mechanism of action - How the drug lowers blood sugar.
- HbA1c reduction - Average change in the key diabetes marker.
- Side‑effect profile - Frequency of GI upset, hypoglycaemia, etc.
- Dosing convenience - Number of pills per day and timing.
- Cost and insurance coverage - Out‑of‑pocket expense for patients.
Side‑by‑Side Comparison Table
| Drug | Mechanism | Typical HbA1c Reduction | Common Side‑effects | Dosing Frequency | Average Monthly Cost (US$) |
|---|---|---|---|---|---|
| Miglitol | Alpha‑glucosidase inhibitor | 0.5-0.7% | Flatulence, abdominal pain, diarrhoea | Three times daily with meals | ≈$45 |
| Acarbose | Alpha‑glucosidase inhibitor (similar to Miglitol) | 0.5-0.8% | Flatulence, diarrhoea, hepatic enzyme elevation (rare) | Three times daily with meals | ≈$40 |
| Voglibose | Alpha‑glucosidase inhibitor (Asian markets) | 0.4-0.6% | Flatulence, abdominal discomfort | Three times daily with meals | ≈$30 |
| Metformin | Biguanide - reduces hepatic glucose production | 1.0-1.5% | GI upset, vitaminB12 deficiency (long‑term) | Once or twice daily (extended‑release) | ≈$10 |
| Sitagliptin | DPP‑4 inhibitor - increases incretin levels | 0.5-0.8% | Nasopharyngitis, headache, rare pancreatitis | Once daily | ≈$150 |
| Glipizide | Sulfonylurea - stimulates pancreatic insulin release | 0.8-1.2% | Hypoglycaemia, weight gain | Once daily (or split dose) | ≈$20 |

Deep Dive into Each Alternative
Acarbose shares Miglitol’s enzyme‑blocking action but is a larger molecule, which can lead to a slightly higher incidence of liver‑enzyme elevations. It’s often chosen when patients cannot tolerate Miglitol’s dose‑related GI symptoms. In practice, the two drugs deliver comparable HbA1c reductions, so the choice hinges on cost and individual tolerance.
Voglibose is popular in Japan, Korea, and China. Its shorter half‑life means it can be taken just before meals, but the drug isn’t widely available in the U.S. or Europe. If you’re practicing in an Asian market, Voglibose can be a budget‑friendly choice, offering similar glucose‑control benefits with a modest side‑effect profile.
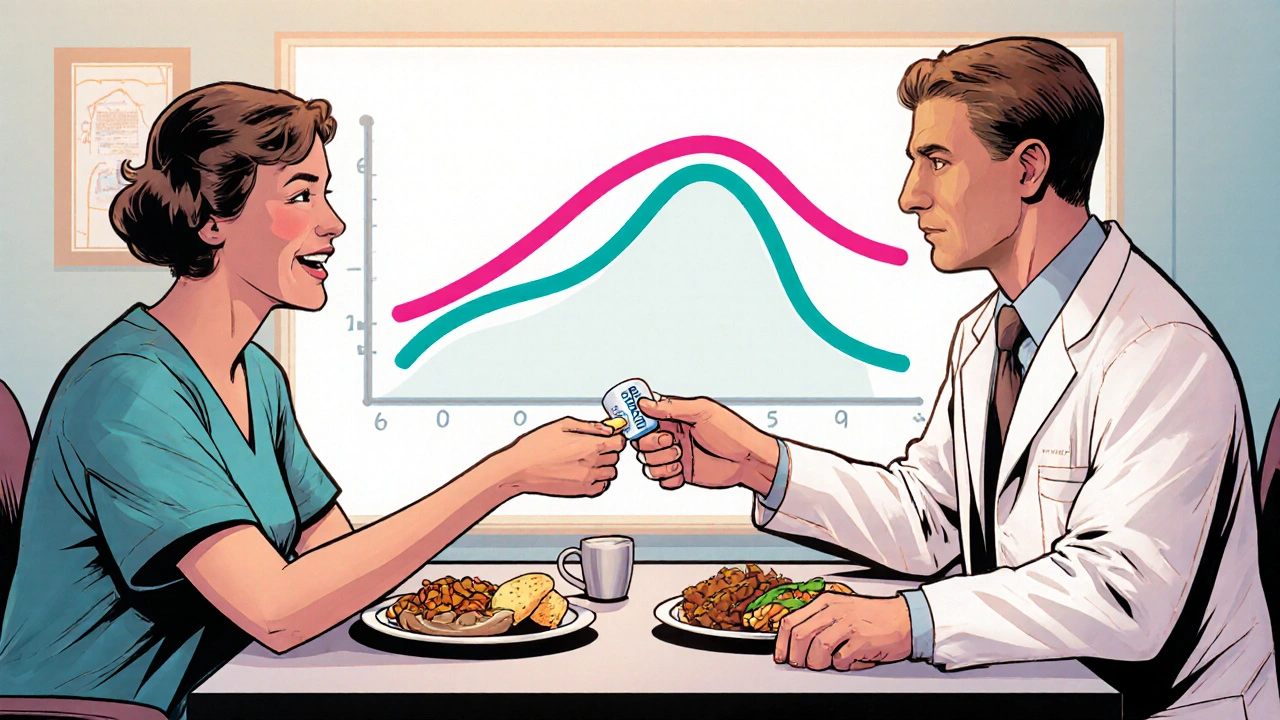
Metformin is the first‑line therapy for almost all patients with type‑2 diabetes. Its ability to lower fasting glucose makes it a stronger HbA1c reducer than Miglitol. However, because it works through a completely different pathway-reducing hepatic glucose output-it doesn’t directly blunt post‑meal spikes the way alpha‑glucosidase inhibitors do. Many clinicians pair Metformin with Miglitol for a synergistic effect on both fasting and post‑prandial glucose.
Sitagliptin (and other DPP‑4 inhibitors) offers a weight‑neutral, low‑hypoglycaemia risk profile. The downside is price: sitagliptin can cost three to four times more than Miglitol, which matters for patients without generous insurance coverage. Its modest HbA1c reduction makes it a good add‑on when other agents have been maximised.
Glipizide belongs to the sulfonylurea class, which forces the pancreas to pump out more insulin. It’s effective at lowering HbA1c, but the risk of hypoglycaemia-especially in the elderly-makes many clinicians hesitant to use it as a first choice. For patients who can tolerate it and need a cheap, once‑daily pill, glipizide remains a viable option.
When Miglitol Is the Right Fit
Miglitol shines for patients who mainly struggle with post‑meal glucose spikes but have relatively stable fasting glucose. It’s also a solid option for those who cannot take metformin due to intolerance or contraindications (e.g., severe renal impairment). Because it’s not absorbed systemically, it has a lower chance of interacting with other oral agents, making it friendly for poly‑drug regimens.
Ideal candidates often share these characteristics:
- Baseline HbA1c 7-9% with noticeable post‑prandial excursions.
- Good renal function (eGFR >60mL/min/1.73m²).
- No history of severe gastrointestinal disease.
- Insurance plans that cover Miglitol at a reasonable copay.
Potential Pitfalls and How to Manage Them
Flatulence and diarrhoea are the most common complaints. Starting at a low dose (25mg) and gradually titrating can ease the gut’s adjustment. Eating a balanced meal with protein and fibre also helps blunt the fermentative side‑effects.
If a patient experiences persistent diarrhoea, consider switching to acarbose or adding a low‑dose probiotic. In rare cases, patients may develop allergic reactions-rash, itching, or swelling-requiring immediate discontinuation.
Practical Tips for Clinicians
- Always counsel patients to take Miglitol with the first bite of each main meal; missing a dose reduces its efficacy.
- Monitor HbA1c after 3 months; if reduction is less than 0.5%, re‑evaluate dose or consider combination therapy.
- Check renal function before initiating; avoid in patients with eGFR <30mL/min/1.73m².
- Review insurance formularies early; a generic version may not be available, affecting out‑of‑pocket cost.
Frequently Asked Questions
Frequently Asked Questions
Can I take Miglitol with Metformin?
Yes. Because Miglitol works in the gut and Metformin works mainly in the liver, they complement each other without significant interaction. Many clinicians start with Metformin as the backbone therapy and add Miglitol to control post‑meal spikes.
Why does Miglitol cause gas?
The drug blocks carbohydrate breakdown, so undigested carbs reach the colon where bacteria ferment them, producing gas. Gradual dose escalation and a diet lower in simple sugars can minimise this effect.
Is Miglitol safe for older adults?
Generally yes, as long as renal function is adequate and the patient can handle the GI side‑effects. Start at the lowest dose and watch for dehydration from diarrhoea.
How quickly does Miglitol lower post‑prandial glucose?
Blood‑glucose peaks are reduced within the first meal after dosing; the full HbA1c benefit becomes evident after 8‑12 weeks of consistent use.
What are the main alternatives if I can’t tolerate Miglitol?
Acarbose and Voglibose are the closest alternatives. If GI issues remain a problem, switching to a DPP‑4 inhibitor like sitagliptin or a biguanide like metformin may be better fits.
Choosing the right diabetes medication isn’t a one‑size‑fits‑all decision. By weighing mechanisms, effectiveness, side‑effects, dosing convenience, and cost, you can match Miglitol-or any alternative-to the patient’s unique needs.
Randy Faulk
October 16, 2025 AT 16:59Understanding the nuanced pharmacodynamics of miglitol can indeed feel labyrinthine; allow me to illuminate the salient points with a touch of eloquence. Miglitol, as an alpha‑glucosidase inhibitor, orchestrates a deceleration of carbohydrate hydrolysis, thereby tempering post‑prandial glycaemic excursions. Its primary virtue lies in its negligible systemic absorption, which confers a modest interaction profile-particularly advantageous for polypharmacy patients. Dosing commences at 25 mg with the inaugural bite of each principal meal, titrating judiciously to a ceiling of 100 mg thrice daily, contingent upon tolerability. Clinicians should vigilantly appraise renal function (eGFR > 60 mL/min/1.73 m²) before initiation, as impaired clearance may exacerbate gastrointestinal adverse events. While its HbA1c decrement hovers around 0.5–0.7 %, the drug’s true merit emerges in patients whose fasting glucose is already well‑controlled yet who endure conspicuous post‑meal spikes. In sum, miglitol occupies a niche where targeted post‑prandial modulation is paramount, especially when metformin is contraindicated.
Brandi Hagen
October 28, 2025 AT 05:46Ah, the glorious intricacies of miglitol! 🌟 Let us embark on an odyssey through the gastrointestinal theater where this agent performs its flamboyant ballet, pirouetting around disaccharide bonds with the poise of a seasoned prima ballerina, all the while casting a veil of flatulence that could rival the most daring of fireworks displays. One must first acknowledge the historic triumph of alpha‑glucosidase inhibition, a triumph that our forebears in pharmacology hailed as a beacon of hope for the post‑prandial warrior. Yet, dear colleagues, the real drama unfolds when patients confront the relentless chorus of bloating, an overture that demands both culinary diplomacy and a titration strategy as delicate as a silk thread. Commencing at a modest 25 mg, the dose can be escalated incrementally, each step accompanied by vigilant monitoring of abdominal symphonies; should the cacophony become intolerable, a strategic retreat to acarbose might be warranted, albeit with its own hepatic overtures. Moreover, the economic recital cannot be ignored-$45 a month may appear modest when juxtaposed against the opulent $150 for a DPP‑4 inhibitor, yet for those besieged by limited insurance fortifications, every penny is a soldier in the battle for adherence. Clinical evidence, drawn from a tapestry of randomized trials, consistently demonstrates a reduction in HbA1c of approximately 0.5 % to 0.7 %, a statistic that, while modest, can be the decisive swing in a tight glycaemic duel. 🩺 In patients with robust renal function, the drug’s destiny shines; however, in the realm of renal impairment, caution transforms from a suggestion to an imperative, lest the kidneys become unwilling accomplices in the pharmacokinetic saga. Let us not forget the synergistic potential when miglitol is paired with metformin-together they orchestrate a symphony that tempers both fasting and post‑prandial glucose, a duet worthy of a standing ovation. Finally, the practitioner’s counsel must be crystal clear: ingest miglitol with the very first bite, for any deviation dilutes its efficacy and turns the therapeutic narrative into a tragic misstep. In this grand theater of diabetes management, miglitol may not claim the leading role, but it certainly delivers a compelling supporting performance that, when cast wisely, enriches the overall production. 🎭
Super Mom
November 8, 2025 AT 19:33Hey mamas! If you’re juggling blood sugar spikes after dinner, miglitol can be a game‑changer. It works right in the gut, so you won’t have to worry about weird drug interactions. Start low, watch the tummy, and pump up the dose if you’re feeling good. Pair it with a solid diet and you’ll see those post‑meal numbers drop. 🙌
debashis chakravarty
November 20, 2025 AT 09:19While the preceding exposition extols miglitol’s virtues, it is incumbent upon us to scrutinize its comparative efficacy against agents such as metformin and sulfonylureas. The incremental HbA1c reduction of merely 0.5–0.7 % may be deemed insufficient for patients whose baseline metrics exceed 9 %. Moreover, the tri‑daily dosing regimen imposes a compliance burden absent in once‑daily therapies. One might argue that the therapeutic index of miglitol is eclipsed by the broader metabolic benefits conferred by metformin, particularly concerning insulin sensitivity and weight modulation. Hence, clinicians should contemplate reserving miglitol for niche scenarios wherein post‑prandial hyperglycaemia predominates and alternative agents prove intolerable.
Daniel Brake
December 1, 2025 AT 23:06In the pursuit of glycaemic equilibrium, we observe that each pharmacologic instrument bears both light and shadow; miglitol, though modest in its HbA1c influence, illuminates the pathway for those seeking to tame the post‑prandial surge without engendering hypoglycaemia.
Suzi Dronzek
December 13, 2025 AT 12:53It is profoundly disheartening to witness the cavalier approach some practitioners adopt when prescribing miglitol, as if the mere act of prescribing a medication absolves them of the duty to educate patients about the inevitable cascade of gastrointestinal disturbances that follow. The expectation that a patient will simply endure flatulence and diarrhoea without a structured mitigation strategy betrays a stark disregard for the sanctity of patient comfort. One must recognize that titration is not a mere number‑crunching exercise; it is an art that demands compassionate dialogue, dietary counseling, and, when necessary, the judicious introduction of a probiotic adjunct. Moreover, the prescriptive reliance on miglitol in lieu of metformin, a drug with a more robust evidence base and superior HbA1c reduction, reflects a myopic focus on post‑prandial metrics at the expense of holistic glycaemic control. To compound the issue, insurance formularies frequently place miglitol behind higher co‑pay barriers, thereby imposing an undue financial strain on patients who are already navigating the labyrinthine complexities of chronic disease management. It is incumbent upon clinicians to weigh these multifaceted considerations with meticulous scrutiny rather than succumbing to the allure of a convenient, albeit limited, therapeutic option. In sum, the prescriber’s responsibility transcends the act of writing a script; it encompasses an unwavering commitment to preemptive education, vigilant follow‑up, and an earnest willingness to pivot when the therapeutic tide proves unfavorable.
Aakash Jadhav
December 25, 2025 AT 02:39Yo fam, miglitol’s like that side‑kick you never asked for but sometimes it saves the day-just don’t forget to take it with your first bite, or it’ll ghost you harder than my last relationship!
Amanda Seech
January 5, 2026 AT 16:26Miglitol can hekp with sugar spikes after meals. It works in the gut and isnt absorbed much. Start low and see how ur tummy feels. If u get too gassy, talk to ur doc.
Lisa Collie
January 17, 2026 AT 06:13One must appreciate that the discussion surrounding miglitol often descends into a populist cacophony, neglecting the nuanced pharmacoeconomic considerations that distinguish it from its counterparts. The modest efficacy, coupled with a tri‑daily dosing requirement, relegates it to a peripheral role in the therapeutic armamentarium, suitable only for a select cohort of patients with pronounced post‑prandial excursions. To elevate the discourse, practitioners should engage with the primary literature and eschew anecdotal endorsements.
rishabh ostwal
January 28, 2026 AT 19:59It would be a grave miscalculation to diminish the significance of miglitol solely on the basis of its modest HbA1c decrement; the drug’s capacity to attenuate post‑prandial hyperglycaemia, when viewed through the prism of cardiovascular risk reduction, commands a more reverent appraisal. Nonetheless, its requirement for thrice‑daily administration imposes a regimen that may erode adherence, a factor that cannot be ignored in the calculus of clinical efficacy. Therefore, while miglitol occupies a legitimate niche, its deployment must be tempered by vigilant patient selection and a readiness to integrate adjunctive modalities should therapeutic goals remain unmet.
Kristen Woods
February 9, 2026 AT 09:46Whilst the clinical data corroborates a modest decrement in HbA1c of approximately 0,5‑0,7 percent, the accompanying gastrointestinal sequelae-namely bloating, flatulunce, and diarrhoea-may prove deterrent for many patients unaccustomed to such adverse effect profiles. Consequently, the prescriber must weigh the trade‑off between glycaemic control and quality of life, especially in a demographic where medication adherence is already fragile.