Ranitidine vs. Popular Alternatives: Benefits, Risks, and How to Choose

Acid Reducer Choice Advisor
Choose Your Medication Based on Symptoms and Needs
Ranitidine is a H2 receptor antagonist that reduces stomach acid production by blocking histamine‑2 receptors on parietal cells. First approved in 1983, it quickly became a go‑to for heartburn, duodenal ulcers, and gastro‑esophageal reflux disease (GERD). However, the 2020 discovery of N‑nitrosodimethylamine (NDMA) contamination forced a worldwide withdrawal, leaving patients and clinicians to hunt for reliable replacements.
TL;DR
- Ranitidine works fast but was recalled due to cancer‑linked NDMA.
- Famotidine and cimetidine are the closest H2 blocker substitutes.
- Proton pump inhibitors (PPIs) such as omeprazole offer longer relief but have different side‑effect profiles.
- Choosing depends on symptom severity, drug interactions, cost, and how quickly you need relief.
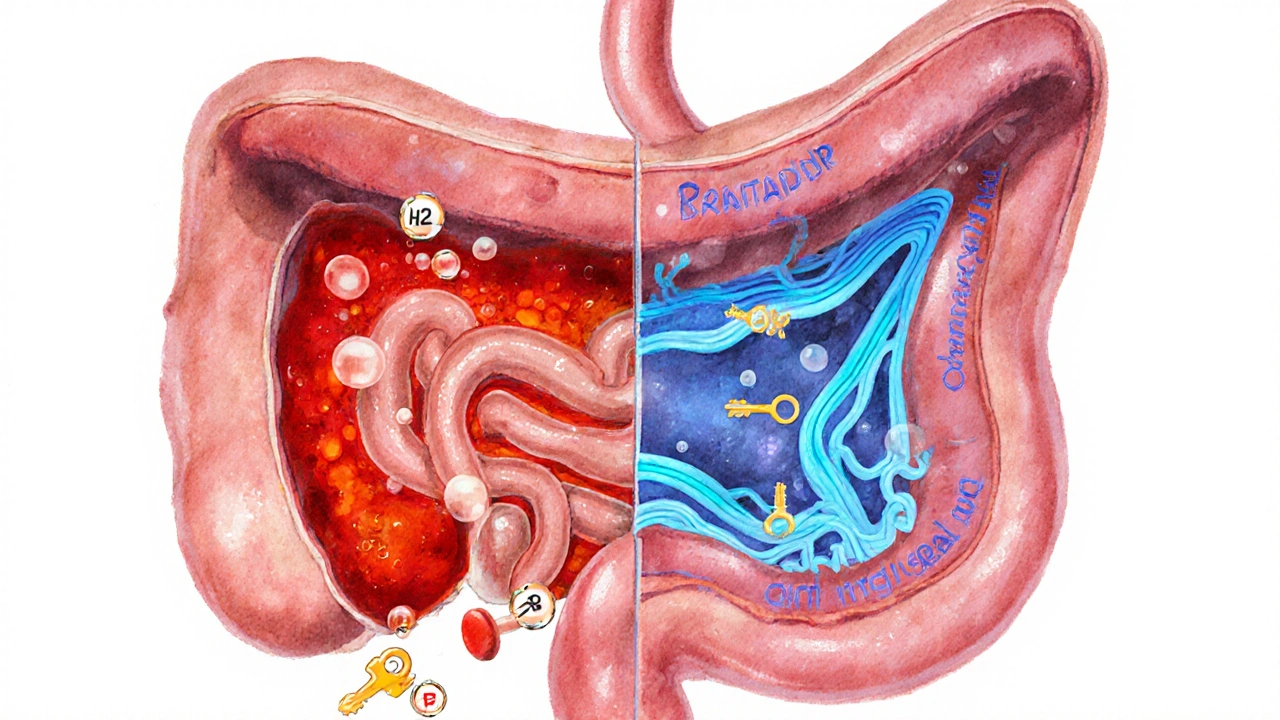
Understanding H2 Blockers
H2 blockers belong to a class of drugs that target the histamine‑2 receptor a protein on stomach lining cells that triggers acid secretion when activated. By preventing histamine from binding, these agents lower the volume of gastric acid without completely shutting it down. Compared with proton pump inhibitors (PPIs), which inhibit the final step of acid production, H2 blockers act earlier in the pathway, giving a quicker onset-usually within 30‑60 minutes.
Ranitidine’s Core Attributes
When it was on the market, ranitidine was favored for its moderate dose range (75‑150mg twice daily) and relatively short half‑life (2‑3hours). This meant patients could take it after meals to curb post‑prandial heartburn. The drug’s low incidence of central nervous system side effects made it a safe choice for older adults, provided the NDMA issue was not a factor.
Major Alternatives to Ranitidine
Below are the most widely used substitutes, each introduced with its own micro‑data block for easy knowledge‑graph extraction.
Famotidine is an H2 receptor antagonist that offers a higher potency than ranitidine, often prescribed at 20‑40mg once or twice daily. Its longer duration (10‑12hours) reduces dosing frequency, and it remained free of NDMA concerns during the 2020 recalls. Cimetidine is another H2 blocker with a dose of 300mg twice daily. While effective, cimetidine is notorious for interacting with cytochromeP450 enzymes, which can boost or blunt the effects of many other medications. Nizatidine is a less common H2 antagonist that mirrors ranitidine’s potency but is only available in a handful of markets, limiting its practical use. Omeprazole is a proton pump inhibitor that blocks the final step of acid production. Typical doses range from 20‑40mg once daily, with an onset of 1‑2hours and a duration extending up to 24hours. Esomeprazole is the S‑isomer of omeprazole, marketed as a slightly more potent PPI. Dosing starts at 20‑40mg daily, and it is often preferred for patients with severe erosive esophagitis.Side‑by‑Side Comparison
| Drug | Class | Typical Dose | Onset | Duration | FDA Status (2025) | Common Side Effects |
|---|---|---|---|---|---|---|
| Ranitidine | H2 blocker | 75‑150mg BID | 30‑60min | 6‑8hr | Withdrawn (NDMA) | Headache, dizziness |
| Famotidine | H2 blocker | 20‑40mg QD/ BID | 30‑60min | 10‑12hr | Available | Diarrhea, constipation |
| Cimetidine | H2 blocker | 300mg BID | 30‑60min | 6‑8hr | Available | Gynecomastia, drug interactions |
| Omeprazole | PPI | 20‑40mg QD | 1‑2hr | 24hr | Available | Headache, nausea, risk of osteoporosis |
| Esomeprazole | PPI | 20‑40mg QD | 1‑2hr | 24hr | Available | Similar to omeprazole, higher cost |
Safety Updates and Regulatory Landscape
The NDMA scare that sidelined ranitidine originated from stability studies showing that, under certain temperature and humidity conditions, the drug degrades into the probable carcinogen. The FDA issued a final recall in October2020 and reinforced testing requirements for all gastric‑acid medicines. Famotidine, cimetidine, and newer PPIs have passed those tests so far, but ongoing surveillance means clinicians must stay alert for any future alerts.
How to Choose the Right Acid‑Reducing Agent
Picking a replacement isn’t a one‑size‑fits‑all decision. Below is a quick decision matrix you can use while talking to your pharmacist or physician.
- Symptom severity: Mild heartburn after meals can be handled with famotidine 20mg after dinner. Moderate to severe reflux often needs a PPI for longer coverage.
- Onset vs. duration: If you need rapid relief, an H2 blocker works faster. For overnight protection, a PPI’s 24‑hour effect is superior.
- Drug interactions: Cimetidine interferes with many cardiac and anti‑seizure meds. If you’re on a complex regimen, famotidine or a PPI is safer.
- Cost and insurance: Generic famotidine and cimetidine are inexpensive; branded PPIs may require a higher copay unless you qualify for a discount program.
- Long‑term safety: Chronic PPI use has been linked to magnesium deficiency and increased risk of certain infections. For chronic, low‑dose use, an H2 blocker may pose fewer systemic concerns.
Step‑by‑Step Guide to Switching from Ranitidine
- Consult your healthcare provider and discuss the reasons for the switch (recall, symptom control, cost).
- Choose the alternative based on the matrix above. For most patients, famotidine is the first‑line H2 blocker.
- Take the first dose of the new drug at the same time you would have taken ranitidine (typically 30minutes before a meal).
- Monitor symptoms for 7‑10days. If heartburn persists, consider stepping up to a PPI under medical guidance.
- Report any new side effects immediately-especially signs of allergic reaction or unusual fatigue.
Related Concepts and Next Topics to Explore
Understanding acid‑related disorders helps you make smarter medication choices. Key related topics include GERD a chronic condition where stomach acid frequently flows back into the esophagus, peptic ulcer disease, H.pylori infection, and lifestyle factors such as diet, body weight, and smoking. After mastering the drug comparison, you might dive deeper into “dietary strategies for GERD” or “when to consider surgical fundoplication.”
Frequently Asked Questions
Why was ranitidine removed from the market?
In 2020 the FDA discovered that ranitidine can form N‑nitrosodimethylamine (NDMA) when exposed to heat or moisture. NDMA is classified as a probable human carcinogen, prompting a voluntary recall and later a mandatory market withdrawal.
Is famotidine as effective as ranitidine?
Clinical studies show famotidine is at least as potent as ranitidine on a milligram‑for‑milligram basis, with a longer duration of action (10‑12hours versus 6‑8hours). Many patients report equal or better symptom control.
Can I take an H2 blocker and a PPI together?
Combining the two is generally unnecessary; a PPI already provides maximal acid suppression. In rare cases, doctors may add an H2 blocker at bedtime to control nocturnal reflux, but this should be supervised.
What side effects should I watch for with cimetidine?
Cimetidine can interfere with the metabolism of drugs that use the cytochromeP450 pathway, leading to higher blood levels of medications like warfarin or theophylline. It may also cause gynecomastia (breast tissue growth) in men.
Are PPIs safe for long‑term use?
Long‑term PPI therapy has been associated with a modest increase in the risk of bone fractures, magnesium deficiency, and certain infections like Clostridioides difficile. Regular monitoring and using the lowest effective dose are recommended.
Mitchell Awisus
September 26, 2025 AT 17:27Thanks for putting together this thorough breakdown, it really helps demystify the landscape of acid‑reducers; the way you charted the onset versus duration is especially handy, and the table makes the data easy to scan, too. I appreciate the nod to NDMA concerns, because safety headlines can get pretty scary, and having clear alternatives listed is a relief. It’s also good to see cost considerations mentioned, since many of us are juggling insurance copays. Overall, solid work-looks like a handy reference for anyone switching from ranitidine.
Annette Smith
October 5, 2025 AT 23:47It’s striking how quickly the market pivoted after the NDMA find, and the article makes that shift feel less confusing. Simple language helps anyone without a medical background understand why famotidine often tops the list now.
beth shell
October 15, 2025 AT 06:07Famotidine generally feels like the safest bet after the ranitidine scare.
khushali kothari
October 24, 2025 AT 12:27The nitrosamine proliferative pathway becomes catalytically favorable under elevated temperature‑humidity matrices, prompting in‑situ N‑nitrosodimethylamine (NDMA) formation via deamination of the dimethylamino side chain of ranitidine. Regulatory pharmaco‑surveillance therefore mandated a Class II recall, obligating manufacturers to substantiate impurity thresholds below the acceptable daily intake of 96 ng. Consequently, therapeutic substitution protocols now prioritize agents with robust degradation profiles, such as famotidine, which exhibits negligible NDMA propensity across the standard stability spectrum. Moreover, the cytochrome P450 interaction index for cimetidine remains a considerable clinical variable, particularly in polypharmacy contexts.
Kelvin Van der Maelen
November 2, 2025 AT 17:47Wow, the whole NDMA drama turned the pharmaceutical world upside‑down-who would’ve thought a heartburn pill could spark such a firestorm?
Jay Jonas
November 12, 2025 AT 00:07hey folks, just a heads up-i switched from ranitidine to famotidine last month and the relief was almost instant. the only thing i noticed was a tiny tummy rumble once in a while, but still way better than the old med. definitely worth a try if you’re looking for a quick fix.
Liam Warren
November 21, 2025 AT 06:27Great rundown! If you’re deciding between an H2 blocker and a PPI, think about how often you need coverage. For occasional heartburn, famotidine’s 12‑hour window usually suffices, while chronic GERD often benefits from the 24‑hour stewardship of omeprazole.
Brian Koehler
November 30, 2025 AT 12:47Dear readers, this comprehensive guide elucidates the pharmacodynamic nuances of acid‑reducing agents; it juxtaposes the rapid onset of H₂ antagonists against the prolonged suppression afforded by proton pump inhibitors, thereby facilitating an informed therapeutic selection. Moreover, the inclusion of cost‑effectiveness analyses herein provides a pragmatic dimension to clinical decision‑making. We commend the authors for integrating safety updates, particularly the NDMA discourse, which remains paramount in contemporary practice.
Dominique Lemieux
December 9, 2025 AT 19:07The withdrawal of ranitidine due to NDMA contamination has undeniably reshaped the therapeutic hierarchy of acid‑reducing medications. While many clinicians initially gravitated toward famotidine as the most straightforward substitution, the broader implications extend beyond mere potency. First, the pharmacokinetic profile of famotidine-characterized by a half‑life of approximately 2.5 hours and a duration of action nearing twelve hours-offers a balance between efficacy and dosing convenience. Second, the drug’s minimal interaction with cytochrome P450 enzymes reduces the risk of adverse drug‑drug interactions, a critical consideration for patients on polypharmacy regimens. Conversely, cimetidine, though pharmacologically comparable, remains a less favorable option due to its notorious inhibition of multiple CYP isoforms, which can precipitate elevated serum concentrations of concomitant medications. Proton pump inhibitors, such as omeprazole and esomeprazole, present a different therapeutic paradigm by irreversibly inhibiting the gastric H⁺/K⁺‑ATPase. Their prolonged acid suppression, lasting up to twenty‑four hours, makes them superior for nocturnal reflux and severe erosive esophagitis. However, the long‑term safety profile of PPIs has attracted scrutiny, with meta‑analyses suggesting associations with bone mineral density loss, hypomagnesemia, and increased susceptibility to enteric infections. Therefore, a risk‑benefit analysis must weigh the immediacy of symptom relief against potential chronic adverse outcomes. From an economic perspective, generic famotidine and cimetidine typically incur lower out‑of‑pocket costs compared with brand‑name PPIs, though formulary negotiations can mitigate this disparity. The decision matrix should also integrate patient‑specific factors such as renal function, as dose adjustments may be requisite for H₂ antagonists in the setting of impaired clearance. Moreover, lifestyle modifications-including weight management, dietary adjustments, and elevation of the head of the bed-remain foundational adjuncts irrespective of pharmacotherapy. Clinicians are encouraged to reassess the necessity of continuous acid suppression, especially in populations at heightened risk for PPI‑related complications. In summary, the optimal replacement for ranitidine is not monolithic; it hinges on individual symptom severity, comorbid conditions, and the patient’s therapeutic priorities. By employing a personalized approach, clinicians can navigate the post‑ranitidine landscape with confidence and safety.
Laura MacEachern
December 19, 2025 AT 01:27It’s encouraging to see that there are safe, affordable options on the market-famotidine, for instance, offers fast relief without the NDMA worries, and many insurers cover it nicely. If you’re unsure, a quick chat with your pharmacist can pinpoint the best fit for your budget and health goals.
BJ Anderson
December 28, 2025 AT 07:47Honestly, the long list of considerations is spot‑on, but the real‑world takeaway is simple: start with famotidine for mild cases and only move up to a PPI if symptoms persist after a week.
Alexander Rodriguez
January 6, 2026 AT 14:07Just to add, the FDA’s latest guidance confirms that all current over‑the‑counter H₂ blockers have passed NDMA testing, so you can pick any of them without fearing hidden contaminants.
Abhinav Sharma
January 15, 2026 AT 20:27Great synthesis! 😊 One thing to remember is that timing matters-taking an H₂ blocker 30 minutes before a meal maximizes its effect, while PPIs are best taken before breakfast for consistent acid control. 💊
Welcher Saltsman
January 25, 2026 AT 02:47Sounds like a solid plan-just hop on famotidine and see how you feel.
april wang
February 3, 2026 AT 09:07When navigating the post‑ranitidine therapeutic landscape, it is useful to adopt a systematic framework that incorporates pharmacodynamic attributes, patient adherence potential, and health‑economic variables. By first categorizing the clinical presentation-whether episodic heartburn, chronic GERD, or ulcer disease-one can align the drug class with the requisite duration and potency. H₂ antagonists, such as famotidine, provide a rapid onset within 30 to 60 minutes, which is advantageous for patients who experience intermittent symptoms tied to specific meals. Their dosing convenience, often limited to once or twice daily, can improve adherence compared to more frequent regimens. In contrast, proton pump inhibitors deliver a profound suppression of gastric acid secretion, extending up to 24 hours, which is essential for severe esophagitis or refractory cases. However, the long‑term safety considerations of PPIs, including potential impacts on bone health and micronutrient absorption, necessitate periodic reassessment. Cost considerations remain pivotal; generic H₂ blockers are typically less expensive, though insurance formularies may favor branded PPIs with co‑pay assistance. Additionally, drug‑drug interaction profiles differ markedly-cimetidine is notorious for CYP450 inhibition, whereas famotidine exhibits minimal interaction risk, making it preferable for polypharmacy patients. Lifestyle modifications-dietary adjustments, weight management, and smoking cessation-should be integrated into any treatment plan to augment pharmacologic efficacy. Ultimately, shared decision‑making, wherein the clinician and patient weigh the benefits, risks, and personal preferences, yields the most sustainable therapeutic outcome.
Vishnu Raghunath
February 12, 2026 AT 15:27Oh sure, because assembling a ten‑step decision tree is exactly what everyone wants when they’re just trying to stop heartburn after a spicy taco.