SSRIs and NSAIDs: Understanding the Elevated Risk of GI Bleeding and How to Prevent It
SSRI and NSAID Risk Assessment Tool
SSRI and NSAID Risk Assessment Tool
Answer a few questions to determine your risk of gastrointestinal bleeding when taking SSRIs and NSAIDs together.
Assess Your Risk
We'll calculate your risk level and provide personalized recommendations based on your answers.
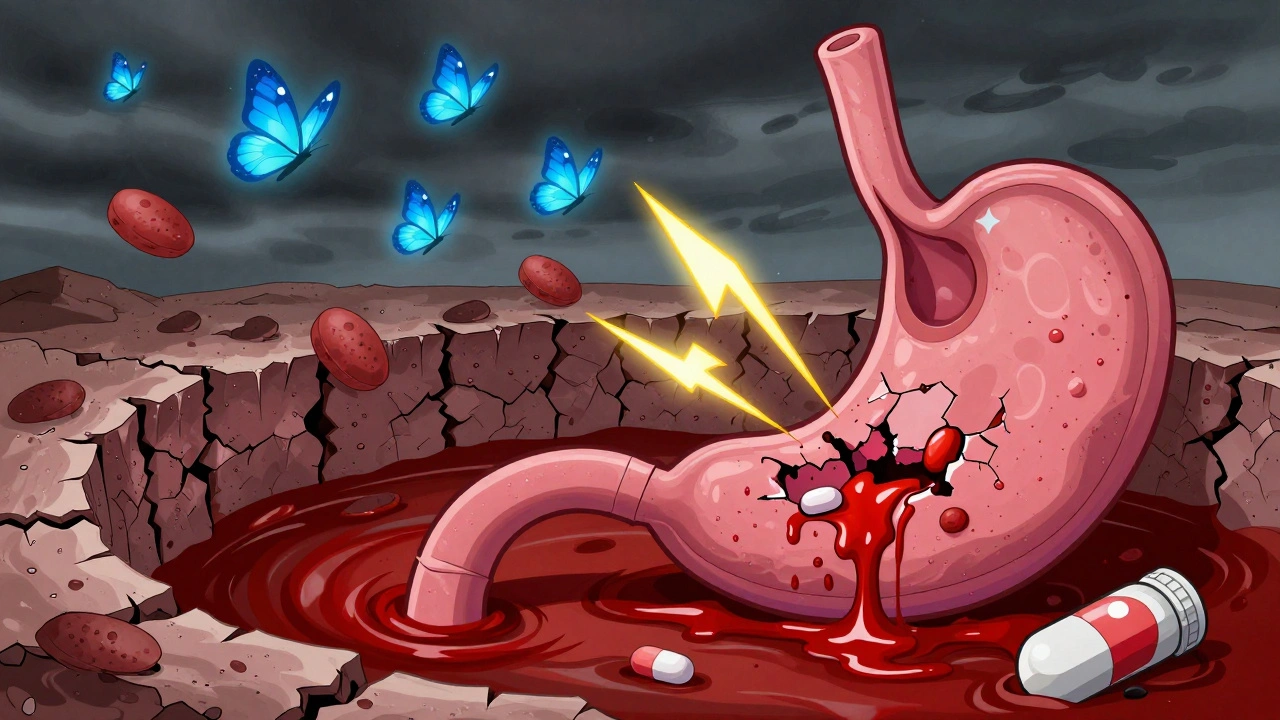
Every year, millions of people take SSRIs for depression or anxiety, and just as many reach for NSAIDs for a sore back, headache, or arthritis pain. Both are common, widely prescribed, and often seen as safe. But when you take them together, something dangerous can happen - your risk of a serious, even life-threatening, gastrointestinal (GI) bleed goes up by 75%. This isn’t a rare side effect. It’s a well-documented, predictable interaction that doctors and patients still overlook far too often.
How SSRIs and NSAIDs Work - and Why They’re Dangerous Together
SSRIs - like sertraline, fluoxetine, and citalopram - work by boosting serotonin in the brain to improve mood. But serotonin isn’t just a brain chemical. It’s also stored in platelets, the blood cells that help stop bleeding. When SSRIs block serotonin reuptake, they also stop platelets from getting the serotonin they need to clump together and form a plug at the site of a cut or ulcer. That means even a small tear in your stomach lining can start bleeding and won’t stop easily. NSAIDs - such as ibuprofen, naproxen, and diclofenac - reduce pain and inflammation by blocking enzymes called COX-1 and COX-2. But COX-1 does more than cause pain; it makes prostaglandins, which protect your stomach lining by keeping mucus flowing and blood circulating. When NSAIDs shut down COX-1, your stomach loses its natural shield. The acid eats away at the tissue, creating ulcers. Combine that with SSRIs slowing down your body’s ability to stop bleeding, and you’ve got a perfect storm. This isn’t just theory. A landmark 2002 study in JAMA Internal Medicine showed that people taking SSRIs had a higher risk of upper GI bleeding. When they added an NSAID, the risk didn’t just go up - it exploded. Later studies, including a 2023 meta-analysis in Digestive Diseases and Sciences, confirmed that the combination increases bleeding risk by 75% compared to using either drug alone. That’s not a small bump. That’s a major jump.Who’s Most at Risk?
Not everyone who takes both drugs will bleed. But some people are far more vulnerable.- People over 65 - aging stomachs produce less mucus and heal slower. The risk of bleeding doubles after age 65.
- Those with a history of ulcers or GI bleeding - if you’ve had one before, your stomach lining is already damaged. Adding SSRIs and NSAIDs is like pouring salt on an open wound.
- People on blood thinners - if you’re also taking warfarin, apixaban, or even low-dose aspirin, your bleeding risk stacks up even higher.
- Those taking high-dose or long-term NSAIDs - daily ibuprofen for months? That’s a red flag. Diclofenac and naproxen carry higher risk than ibuprofen.
One 2021 survey of over 1,200 primary care doctors found that fewer than 25% of them routinely checked for this interaction before prescribing. That means a lot of patients are being put at risk without even knowing it.
Which NSAIDs Are Safer? Which SSRIs Are Riskier?
Not all NSAIDs are created equal. Some are harder on your stomach than others.| Medication Type | Example | Relative Risk of GI Bleeding (OR) |
|---|---|---|
| Non-selective NSAID (high risk) | Naproxen, Diclofenac | 3.5-4.0 |
| Non-selective NSAID (lower risk) | Ibuprofen | 2.0-2.5 |
| Selective COX-2 inhibitor | Celecoxib | 1.16 |
| SSRI (monotherapy) | Fluoxetine, Sertraline | 1.4-1.5 |
| SSRI + NSAID (combination) | Any SSRI + any NSAID | 1.75 |
Celecoxib is the clear winner among NSAIDs when it comes to GI safety. It doesn’t block COX-1 much, so it leaves your stomach lining mostly protected. If you’re on an SSRI and need pain relief, celecoxib is the safest NSAID option - if you can tolerate it.
Among SSRIs, most carry similar bleeding risks because they all affect platelet serotonin. But some data suggests escitalopram may be slightly safer than fluvoxamine or paroxetine. That’s not a reason to switch unless you’re having side effects - but it’s worth noting if your doctor is choosing between options.

What to Do If You’re Taking Both
If you’re already on an SSRI and an NSAID, don’t panic. But do take action.- Ask your doctor if you really need both. Can your pain be managed with acetaminophen (paracetamol)? It doesn’t affect platelets or stomach lining. For chronic pain, physical therapy, heat packs, or even low-dose antidepressants like amitriptyline (which also helps with nerve pain) might be better options.
- If you must take both, get a proton pump inhibitor (PPI). Medications like omeprazole, esomeprazole, or pantoprazole reduce stomach acid and help your lining heal. Studies show PPIs cut the extra bleeding risk from SSRIs and NSAIDs by about 70%. A daily 20mg dose of omeprazole is usually enough.
- Get tested for H. pylori. This bacteria causes most ulcers. If you have it, treating it can reduce your bleeding risk by half. The American College of Gastroenterology now recommends testing before starting dual therapy for high-risk patients.
- Watch for warning signs. Black, tarry stools? Vomiting blood? Sudden dizziness or weakness? These aren’t normal. Call your doctor or go to the ER immediately.
One patient on Reddit shared that after switching from naproxen to celecoxib and adding omeprazole, they had no GI issues for over a year while staying on sertraline. That’s not luck - that’s smart management.
Why This Keeps Happening - And How Systems Are Changing
You’d think doctors would know this. But a 2022 Medscape survey found that 68% of patients weren’t warned about this risk when prescribed both drugs. Part of the problem is time. A doctor’s visit lasts 10-15 minutes. It’s easy to miss drug interactions when you’re juggling depression, arthritis, high blood pressure, and diabetes. But hospitals are catching on. Since 2019, major systems like Cleveland Clinic have added automated alerts in their electronic records. When a doctor tries to prescribe an SSRI and NSAID together, the system pops up a warning and suggests a PPI. Since then, GI bleeding admissions in dual-therapy patients have dropped by 42%. The FDA and European Medicines Agency both added warnings to SSRI labels in 2019-2020. But warnings alone don’t change behavior. Real change comes from systems - alerts, guidelines, and better patient education.
What’s Next? New Solutions on the Horizon
Researchers aren’t just warning - they’re building solutions.- Combination pills - TissueTech is testing a pill that releases ibuprofen and omeprazole together. It’s still in trials, but early results look promising.
- Genetic testing - Some people metabolize PPIs slowly because of their CYP2C19 gene. Testing for this could help doctors pick the right dose or drug.
- AI risk predictors - A 2023 study used machine learning to analyze EHR data and predict bleeding risk with 86% accuracy. Imagine a system that flags your risk before you even get the prescription.
Dr. Amy Foxx-Orenstein, past president of the American College of Gastroenterology, says we’re approaching a tipping point: “Concomitant SSRI and NSAID prescribing without gastroprotection will be considered negligent care for most adult patients.” That’s not an exaggeration. It’s the new standard.
Bottom Line: Don’t Assume It’s Safe
SSRIs and NSAIDs are not harmless. Together, they create a hidden danger that many patients and providers still ignore. But you don’t have to be part of the statistic.- If you’re on an SSRI and take NSAIDs for pain - talk to your doctor about alternatives.
- If you must take both - ask for a PPI. Don’t wait for symptoms.
- If you’ve had a GI bleed before - avoid NSAIDs entirely unless absolutely necessary.
- If you’re over 65 - treat this combination like a red flag, not a routine prescription.
This isn’t about fear. It’s about awareness. You have the right to know what’s in your body and what it might do. And you have the power to ask the right questions - before it’s too late.
Can I take ibuprofen with sertraline?
You can, but it increases your risk of upper GI bleeding by about 75% compared to taking either drug alone. If you need pain relief while on sertraline, talk to your doctor about switching to acetaminophen or using celecoxib instead. If you must use ibuprofen, always take a proton pump inhibitor like omeprazole at the same time to protect your stomach lining.
What are the signs of a GI bleed from SSRIs and NSAIDs?
Watch for black, tarry stools (called melena), vomiting blood or material that looks like coffee grounds, sudden dizziness, fainting, rapid heartbeat, or unexplained weakness. These are emergency signs. Don’t wait - go to the ER immediately if you experience any of them.
Are all SSRIs equally risky for GI bleeding?
Most SSRIs carry similar bleeding risks because they all interfere with platelet serotonin. However, some studies suggest escitalopram may have a slightly lower risk than fluvoxamine or paroxetine. Still, the difference is small, and switching SSRIs isn’t usually the best solution - focusing on reducing NSAID use or adding a PPI is more effective.
Is celecoxib safe to take with SSRIs?
Yes, celecoxib is the safest NSAID option when combined with SSRIs. It doesn’t significantly block the COX-1 enzyme that protects your stomach, so it carries much less bleeding risk than naproxen or ibuprofen. Studies show its risk is close to baseline - only 16% higher than not taking any NSAID. Still, adding a PPI is recommended for high-risk patients, like those over 65 or with a past ulcer history.
How long should I take a PPI if I’m on both an SSRI and NSAID?
If you’re taking both medications long-term, you should take a PPI daily for as long as you’re on the combination. Stopping the PPI even briefly can leave you vulnerable. If you eventually stop the NSAID, you can usually stop the PPI too - but always check with your doctor first. For short-term NSAID use (a few days), a short course of PPI may be enough.
Can I switch to a different antidepressant to avoid this risk?
Yes. Bupropion (Wellbutrin) is an antidepressant that doesn’t affect platelet serotonin, so it doesn’t increase GI bleeding risk. If you’re on an SSRI and need to stay on NSAIDs, bupropion might be a good alternative - but only if it’s appropriate for your depression symptoms. Talk to your doctor about whether switching makes sense for you.
Reshma Sinha
December 11, 2025 AT 13:44Wow, this is such an important post. I work in pharma analytics and we see this interaction all the time-especially in elderly patients on multiple meds. The 75% increase isn't just a number, it's real people ending up in the ER. We need better EHR alerts and patient handouts. PPIs should be auto-suggested when SSRIs and NSAIDs are co-prescribed. Simple. Effective. Life-saving.
sandeep sanigarapu
December 13, 2025 AT 09:30Take both? Bad idea. Use acetaminophen. Add PPI if needed. Simple.
Audrey Crothers
December 14, 2025 AT 03:35Thank you for posting this!! 😊 I'm on sertraline and was taking ibuprofen for my back-didn't know this was a thing. My doctor just prescribed me omeprazole yesterday and I feel like I just got a superpower. Please, if you're on SSRIs and pain meds, read this and talk to your doc. You're not being paranoid-you're being smart. 💪
Robert Webb
December 15, 2025 AT 06:11There's a deeper systemic issue here. Medical education still treats drug interactions as an afterthought-something you memorize for exams, not something you live with daily. Primary care doctors are overworked, underpaid, and drowning in clinical decision fatigue. That’s why automated alerts in EHRs are not a luxury-they’re a necessity. And yet, many clinics still use outdated systems. The fact that Cleveland Clinic saw a 42% drop in GI bleeds after implementing alerts proves that tech can save lives. We need this everywhere, not just in academic centers. It’s not about blaming doctors-it’s about building systems that make the right choice the easy choice.
Adam Everitt
December 16, 2025 AT 16:41hmm… so ssris mess w/ platelets… and nsaids mess w/ stomach… so combo = bad… but what if u take celecoxib + ppi? is that just… avoiding the problem? or is it actually solving it? i mean, if we’re just patching the leak instead of fixing the pipe…
Levi Cooper
December 18, 2025 AT 02:03Wow, another one of these ‘medical alarmist’ posts. You act like SSRIs are poison. My cousin’s been on fluoxetine for 12 years and takes ibuprofen every day-he’s fine. People need to stop being hysterical. This isn’t a crisis, it’s a statistical blip. You’re scaring people out of needed meds. Maybe if you stopped eating junk food and exercised, you wouldn’t need NSAIDs in the first place.
Ashley Skipp
December 19, 2025 AT 18:06Everyone’s freaking out over a 75% increase but you’re ignoring the baseline. Most people won’t bleed. And if they do, it’s rare. Why are you making healthy people paranoid? I’ve been on sertraline and naproxen for 5 years. No issues. Stop fearmongering.
Nathan Fatal
December 21, 2025 AT 12:24Levi, your comment is dangerously misleading. The 75% increase is relative, but the absolute risk for a healthy 30-year-old is still under 0.5% per year. The danger is real for high-risk groups-elderly, history of ulcers, on anticoagulants-but dismissing the data because ‘my cousin is fine’ ignores epidemiology. This isn’t fearmongering-it’s harm reduction. The FDA and ACG didn’t issue warnings because they’re paranoid. They did it because the data is robust. Your attitude is exactly why this problem persists.
Stacy Foster
December 21, 2025 AT 16:31Wait… so the FDA added warnings in 2019… and now hospitals have alerts… but who funded those alerts? Big Pharma? Who profits from PPIs? Omeprazole is a billion-dollar drug. Are we being manipulated into lifelong PPI use so corporations can sell more pills? This feels like a scheme. Why not just stop prescribing SSRIs? Maybe depression isn’t a real illness anyway. Maybe it’s just weakness.
nikki yamashita
December 22, 2025 AT 07:43Y’all are overcomplicating this. If you’re on an SSRI and need pain relief, try heat, stretching, or even acupuncture. If you still need meds, go with Tylenol. If you’re in chronic pain, talk to a PT. No need to risk bleeding. Simple, safe, and free. 💕
Donna Anderson
December 22, 2025 AT 11:39i just found out my dad had a bleed last month and he was on citalopram + naproxen for his arthritis… he’s ok now but it was scary as hell. why didn’t his dr tell him? he’s 72. i’m so mad. thanks for this post. i’m printing it out and taking it to his next appt.
Rob Purvis
December 24, 2025 AT 07:49One thing missing from this: What about people who take NSAIDs occasionally? Like, ibuprofen once a week for a headache? The risk is still elevated, but is it clinically meaningful? And what about low-dose aspirin? It’s an NSAID too-but it’s cardioprotective. Do we stop aspirin? No. Do we avoid SSRIs? No. So what’s the balanced approach? I think the answer is: assess individual risk, then tailor. For a 68-year-old with a history of ulcers? Avoid NSAIDs entirely. For a 40-year-old with no history and occasional use? Acetaminophen is still better, but occasional ibuprofen with a PPI is reasonable. Context matters. Don’t treat this like a binary rule.
Lawrence Armstrong
December 26, 2025 AT 06:03Just wanted to add-my GI doc put me on esomeprazole 20mg daily when I started sertraline. I’ve been on both for 3 years. No issues. Also, I take celecoxib for my knee. Zero GI symptoms. The key? Consistency. Don’t skip your PPI. Don’t take NSAIDs ‘only when it hurts.’ If you’re on the combo, treat it like a chronic regimen. Also, if you’re on a PPI, get your B12 and magnesium checked yearly. Long-term PPIs can cause deficiencies. It’s not magic-it’s management. 🧠
wendy b
December 27, 2025 AT 11:01While I appreciate the clinical rigor of this post, I must note that the reliance on PPIs introduces a cascade of unintended consequences: microbiome disruption, increased risk of C. diff, potential nutrient malabsorption, and rebound acid hypersecretion upon discontinuation. Furthermore, the notion that celecoxib is ‘safe’ ignores its cardiovascular risks, which are well-documented in the COX-2 inhibitor class. The real solution lies not in pharmacological patchwork, but in holistic, non-pharmacological pain and mood management. We have regressed into a pill-for-every-problem culture. The data is clear-but the paradigm is broken.