Therapeutic Interchange: What Providers Really Do When Switching Medications Within the Same Class
When a doctor prescribes a medication and the pharmacy gives you a different one, it’s natural to wonder: Why? Did they make a mistake? Is this cheaper? Is it safe? Many people assume the switch is between completely different types of drugs-like swapping a blood pressure pill for a diabetes one. But that’s not what therapeutic interchange actually means. In reality, it’s a carefully controlled process that happens within the same drug class, not across different ones. And it’s not something pharmacists do on their own. It’s a team decision, backed by evidence, and designed to keep patients safe while cutting costs.
Therapeutic Interchange Isn’t What Most People Think
Let’s clear up the biggest misunderstanding right away: therapeutic interchange does not mean switching from one drug class to another. You won’t see a pharmacist swap lisinopril (an ACE inhibitor) for metformin (a diabetes drug). That would be dangerous-and illegal. Instead, therapeutic interchange means replacing one drug with another in the same class that works similarly. For example, switching from atenolol to metoprolol, both beta-blockers used for high blood pressure. Or swapping simvastatin for rosuvastatin, two statins for cholesterol. The goal isn’t to treat a different condition. It’s to get the same result with a drug that’s more affordable, better tolerated, or more available.
This isn’t guesswork. It’s based on years of clinical data. The American College of Clinical Pharmacy defines therapeutic interchange as replacing a prescribed drug with another that’s chemically different but has substantially equivalent clinical outcomes. That means studies show both drugs work just as well for the same condition. Hospitals and long-term care facilities have used this approach since at least 2002, with over 80% of U.S. hospitals having formal programs by then.
Who Decides What Gets Swapped?
It’s not the pharmacist. It’s not the doctor alone. It’s a committee. Every major hospital, nursing home, or healthcare system that uses therapeutic interchange has a Pharmacy and Therapeutics (P&T) Committee. This group includes pharmacists, physicians, nurses, and sometimes even patient advocates. They meet regularly to review which drugs belong on the facility’s formulary-the official list of approved medications.
When a new drug comes out, they compare it to existing options. Is it just as effective? Does it have fewer side effects? Is it significantly cheaper? If the answer is yes on all three, they may add it to the formulary and authorize therapeutic interchange. For example, if a hospital’s formulary includes both generic and brand-name versions of a drug, they might decide that the generic is just as good and should be used by default unless there’s a specific reason not to.
These decisions aren’t made in isolation. They’re based on published clinical trials, real-world outcomes data, and cost analyses. A 2018 study from the National Library of Medicine showed that therapeutic interchange programs can save skilled nursing facilities tens of thousands of dollars each month on pharmacy bills-without lowering patient care quality.
How It Actually Works in Practice
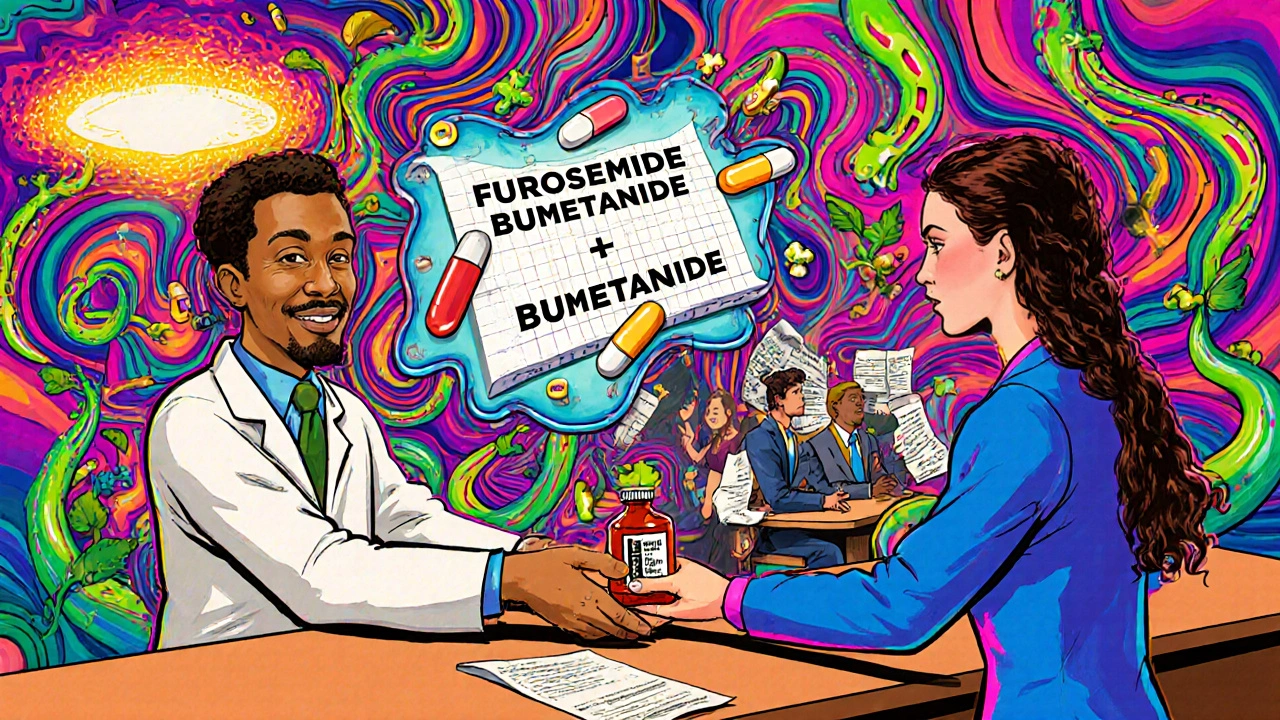
Here’s how it plays out on the ground. A patient is admitted to a hospital with heart failure. The admitting doctor prescribes furosemide, a common diuretic. But the hospital’s formulary lists bumetanide as the preferred option because it’s equally effective, has a longer duration of action, and costs 40% less. The pharmacist checks the formulary, confirms bumetanide is approved for interchange, and dispenses it instead.
But here’s the catch: the pharmacist doesn’t just swap it and move on. They document the change and notify the prescribing doctor. In many cases, especially in long-term care, the prescriber must sign a Therapeutic Interchange (TI) letter upfront. This document says, “I agree that for this patient, if furosemide is prescribed, bumetanide can be substituted without calling me again.” Once that’s on file, the pharmacy can make the switch automatically every time.
In community pharmacies, it’s different. Outside of institutional settings, pharmacists rarely make these swaps without first calling the prescriber. State laws vary, but most require direct approval before changing a medication-even within the same class. That’s why you might get the exact drug your doctor ordered, even if a cheaper alternative exists. The system is designed to protect patients from unintended changes, especially when care is fragmented across multiple providers.
Why This Matters for Patients
Therapeutic interchange isn’t just about saving money for hospitals. It’s about making treatment more consistent and predictable. When a nursing home uses a standardized formulary, every resident gets the same evidence-based options. That reduces confusion. It cuts down on medication errors. And it helps staff manage complex drug regimens more safely.
Patients benefit too. If a drug causes nausea or dizziness, and there’s a better-tolerated alternative in the same class, therapeutic interchange gives providers a legal, safe way to switch without restarting the whole prescription process. It also helps patients who struggle with cost. A statin like rosuvastatin might be $20 a month, while a generic version costs $5. Switching can mean the difference between taking the medicine or skipping doses.
But there’s a flip side. If the interchange isn’t done carefully, it can backfire. Not all drugs in the same class are created equal. For example, switching from one beta-blocker to another might be fine for high blood pressure, but if the patient has asthma, certain beta-blockers could trigger breathing problems. That’s why P&T committees build in exceptions. They don’t just say “swap everything.” They say, “Swap unless the patient has kidney disease, is over 80, or is on another interacting drug.”
Where It Works Best-and Where It Doesn’t
Therapeutic interchange shines in places where care is centralized: hospitals, nursing homes, VA facilities, and large clinics with integrated electronic records. These settings have the infrastructure to track formulary rules, document changes, and communicate across teams.
It struggles in community pharmacies, especially where prescribers are spread out and electronic systems don’t talk to each other. A patient might get their blood pressure medication from a local pharmacy, see their cardiologist at a different clinic, and get diabetes care at a community health center. In that case, automatic substitution is too risky. Pharmacists there usually have to call the prescriber for approval-adding time and friction to the process.
It also doesn’t work well for drugs with narrow therapeutic windows, like warfarin or lithium. Even small changes in dose or formulation can lead to serious side effects. These drugs are typically excluded from interchange programs altogether.
The Bottom Line: Safety First, Savings Second
Therapeutic interchange is a smart, proven tool-but only when done right. It’s not a loophole to cut corners. It’s a structured, evidence-based process that puts patient safety at the center. The goal isn’t to swap drugs for the sake of saving money. It’s to use the best available option that delivers the same outcome at a lower cost.
For patients, the key is to ask questions. If you get a different pill than what your doctor wrote, ask: “Is this the same kind of medicine? Is it safe for me? Did my doctor approve this?” Most providers are happy to explain. And if you’re on a long-term medication, ask if your care team uses a formulary. You might be surprised to learn that your pharmacy is following a carefully designed plan-not just picking the cheapest option.
For providers, the lesson is clear: therapeutic interchange works best when it’s collaborative, documented, and grounded in clinical evidence. It’s not a shortcut. It’s a system. And when done well, it helps patients stay healthy-and keeps healthcare affordable.
Is therapeutic interchange the same as generic substitution?
No. Generic substitution means replacing a brand-name drug with its chemically identical generic version-same active ingredient, same dose, same manufacturer (just cheaper). Therapeutic interchange means swapping a drug for a different one in the same class-like switching from one statin to another-that has similar effects but isn’t chemically identical. Generics are exact copies. Interchanges are alternatives.
Can a pharmacist make a therapeutic interchange without the doctor’s approval?
In most cases, no. In hospitals or long-term care facilities with formal programs, pharmacists can make the switch if it’s pre-approved by the Pharmacy and Therapeutics Committee and the prescriber has signed a TI letter. In community pharmacies, pharmacists almost always need to contact the prescriber first. State laws vary, but patient safety rules generally require direct communication before changing a prescribed medication-even within the same class.
Why don’t all doctors support therapeutic interchange?
Some doctors worry that swapping medications-even within the same class-could lead to unexpected side effects or reduced effectiveness. Others feel it undermines their authority. But research shows that when done properly, with input from pharmacists and clear guidelines, therapeutic interchange improves outcomes and reduces costs. The biggest barrier isn’t clinical-it’s communication. Many providers aren’t trained on how these programs work or don’t know how to opt in.
Are there drugs that should never be interchanged?
Yes. Drugs with narrow therapeutic windows-like warfarin, digoxin, lithium, and some seizure medications-are usually excluded because small differences in absorption or metabolism can cause serious harm. Also, drugs used for conditions that require precise dosing, like thyroid replacement or psychiatric medications, are often kept on a separate list and not subject to interchange. P&T committees carefully review each drug before allowing substitutions.
Does therapeutic interchange affect how well my medication works?
If the interchange follows evidence-based guidelines, it shouldn’t. The whole point is to choose a drug that has been proven to work just as well. Studies from hospitals and nursing homes show no drop in effectiveness when switching between approved alternatives. But if the swap isn’t based on solid data-or if your individual health needs aren’t considered-then yes, it could affect outcomes. That’s why patient-specific factors like age, kidney function, allergies, and other medications are always checked before a switch.
Tina Dinh
December 1, 2025 AT 10:55OMG this is such a relief to read! 🙌 I thought my pharmacist was just cutting corners, but now I get it-this is actually smart, science-backed stuff. My grandma’s on a statin swap and she’s never felt better. 💪
Bernie Terrien
December 1, 2025 AT 21:33Pharma’s Trojan horse. Cost-cutting dressed as ‘clinical equivalence.’ They swap because they can, not because they should. Trust the algorithm, not the doctor.
Peter Axelberg
December 3, 2025 AT 15:51Man, I’ve been on this ride for years. Got switched from atenolol to metoprolol after a hospital stay-thought I was getting screwed. Turns out, my BP’s been rock-solid since. No more dizziness, cheaper script, same results. The system ain’t perfect, but it’s not the villain everyone thinks it is.
And yeah, I know some folks get screwed-especially if they’re on 12 meds and their docs don’t talk to each other. But that’s a fragmentation problem, not an interchange problem. Fix the EHRs, not the policy.
Sara Shumaker
December 5, 2025 AT 03:29It’s fascinating how we’ve turned healthcare into a chess game of formularies and committees. The real question isn’t whether interchange works-it’s who gets to decide what ‘equivalent’ means. Is it the pharmacist? The insurer? The hospital CFO? The patient? We say it’s evidence-based, but evidence is always filtered through power. Who’s excluded from the conversation when they draft those TI letters?
I’ve seen elderly patients nodding along because they’re too tired to ask. That’s not safety. That’s surrender.
linda wood
December 6, 2025 AT 10:18So let me get this straight-you’re telling me my doctor didn’t *actually* prescribe the pill I got? And that’s… okay? 😏
Mary Kate Powers
December 6, 2025 AT 13:50As a nurse who’s seen this play out in long-term care, I can tell you: when done right, this saves lives. One resident kept missing doses because her brand-name med cost $120/month. Switched to a generic statin-same efficacy, $5. She’s been compliant for 3 years now. No adverse events. No drama. Just better health.
And yes, we have protocols. We check kidney function, drug interactions, allergies. We don’t just swap blindly. This isn’t some backroom scheme. It’s clinical teamwork.
Scott Collard
December 6, 2025 AT 21:53Of course it’s ‘evidence-based.’ The evidence is funded by the manufacturers pushing the cheaper drug. Wake up. This isn’t medicine-it’s supply chain optimization disguised as care.
jamie sigler
December 8, 2025 AT 15:49So I’m supposed to be grateful my blood pressure med got swapped without me being asked? Cool. I’ll just sit here quietly while they play doctor with my body. 🤡
Peter Lubem Ause
December 9, 2025 AT 16:25Let me break this down for those who think this is a conspiracy: therapeutic interchange isn’t about replacing your medicine-it’s about replacing the *cost* of your medicine with something that works just as well. And when you’re talking about a 78-year-old on fixed income, that’s not cruelty, it’s compassion.
Yes, some drugs shouldn’t be swapped-warfarin, lithium, seizure meds. That’s why P&T committees exist. They’re not robots. They’re clinicians reviewing real data. If you’re scared of interchange, you’re scared of *systems*. But systems aren’t evil-they’re just poorly implemented. Fix the communication gaps, not the concept.
I’ve worked in Nigerian public hospitals where patients pay out of pocket for *every* pill. Here, we have formularies that prevent people from choosing between food and medicine. That’s not a flaw. That’s progress.
Jennifer Wang
December 10, 2025 AT 18:18It is imperative to underscore that therapeutic interchange protocols must adhere strictly to the American College of Clinical Pharmacy guidelines, particularly regarding pharmacokinetic and pharmacodynamic equivalence. Deviations from evidence-based formulary standards constitute a breach of professional duty and may expose institutions to liability. Furthermore, documentation via signed TI letters must be maintained in the electronic health record with timestamped audit trails to ensure regulatory compliance and patient safety.
stephen idiado
December 12, 2025 AT 00:58Interchange? More like corporate coercion. You think this is clinical? It’s actuarial. They swap because the actuary says so. Not because the patient needs it. The data? Manufactured. The outcomes? Anecdotal. The real goal: reduce cost per QALY. Not improve life.
Subhash Singh
December 13, 2025 AT 01:02While the conceptual framework of therapeutic interchange is commendable, one must critically evaluate the generalizability of formulary decisions across heterogeneous populations. For instance, genetic polymorphisms in CYP450 enzymes may render certain statin substitutions suboptimal in South Asian populations. Are these pharmacogenomic variables adequately considered in P&T committee deliberations? The literature remains inconclusive.
Geoff Heredia
December 14, 2025 AT 07:45Ever notice how every time a drug gets swapped, the price drops and the CEO gets a bonus? Coincidence? I think not. This isn’t about safety-it’s about hiding profit margins behind a white coat. The FDA doesn’t regulate interchange. The insurers do. And they don’t care if you get a rash. They care if the stock goes up.
Andrew Keh
December 14, 2025 AT 17:36I appreciate the clarity here. It’s easy to panic when you get a different pill. But knowing there’s a team checking the science, documenting the change, and prioritizing safety… that’s reassuring. I wish more people understood this wasn’t random-it’s intentional, thoughtful work.
Matthew Higgins
December 16, 2025 AT 08:36So I get it now. My pharmacist didn’t mess up. They were following a plan. And honestly? I kinda love that. I used to think I was being cheated. Turns out, I was just… unaware.
My buddy in Chicago got switched from one beta-blocker to another and ended up with way fewer side effects. He didn’t even notice until his wife pointed out he wasn’t falling asleep at dinner anymore.
It’s wild how much of medicine happens behind the scenes. We think it’s just the doctor and the pill. But there’s a whole crew-pharmacists, nurses, committees-working to keep us alive while keeping costs down. Not sexy. But vital.
Still… I wish they’d just *tell* us. A little note on the bottle: ‘This is a therapeutic interchange. Approved by your care team.’ That’s all it takes to turn fear into trust.