What Each Part of Your Rx Medication Label Means for Patients

Every time you pick up a prescription, you get a little white or yellow label stuck to the bottle. It looks simple-just a few lines of text. But if you don’t know what each part means, you could be taking your medicine wrong. And that’s not just risky-it’s dangerous. Around 1.5 million medication errors happen in the U.S. every year, and many of them come from patients misunderstanding their labels. You don’t need to be a pharmacist to read it. You just need to know what each piece is telling you.
Your Name Is on There for a Reason
The very first thing you see is your full name. It’s not just for show. This is your safety net. Pharmacies fill hundreds of prescriptions a day. A mix-up between "John Smith" and "Jon Smith" can happen. That’s why your name is printed clearly at the top. If you see someone else’s name, don’t take it. Even if the pill looks the same. A 2023 Cleveland Clinic study found that 12% of medication errors in older adults happened because someone grabbed the wrong bottle-usually because they didn’t check the name first.
Brand Name vs. Generic Name
You’ll see two names for your medicine. One is the brand name-like "Abstral"-and the other is the generic name-"fentanyl." The brand name is what the company calls it when they sell it. The generic name is the actual drug inside. They’re the same thing. But knowing the generic name helps you spot duplicates. For example, if your doctor prescribes "Lipitor" and your insurance switches you to "atorvastatin," you’re still getting the same medicine. If you don’t know the difference, you might think you’re being given something new-and refuse it. Or worse, you might take both and overdose.
Dosage: What Each Pill or Drop Contains
This part tells you how strong your medicine is. It might say "10 mg" or "500 mcg." That’s the amount of active ingredient in each pill, capsule, or drop. If your label says "take one tablet daily" and the dosage is "10 mg," you’re taking 10 milligrams each day. If your doctor changes your dose to 20 mg, your new label should reflect that. Never guess. If the number looks wrong-like you used to take 5 mg and now it’s 50 mg-call your pharmacist. A 2022 study in JAMA Internal Medicine showed that 22% of dosing errors happened because patients didn’t realize the strength had changed.
How and When to Take It
This is the most important instruction. It tells you how often to take the medicine and under what conditions. "Take one tablet by mouth every 8 hours" means three times a day, spaced evenly. "Take with food" means don’t swallow it on an empty stomach-some drugs cause nausea if you do. "Take on an empty stomach" means wait at least an hour before or two hours after eating. "Take at bedtime" helps you remember and avoids daytime drowsiness. If your label says "as needed," that means only take it when you feel the symptom-like pain or nausea-not every day. Confusing "every 4 hours" with "four times a day" is a common mistake. One is every 4 hours around the clock. The other is morning, noon, evening, bedtime. Mixing them up can lead to overdose.
Expiration Date: When It Stops Working
That date on the label isn’t arbitrary. It’s the last day the manufacturer guarantees the drug will work as intended. After that, it might not be as strong-or it could break down into something harmful. Most pills last 12 to 18 months after being filled. Liquid antibiotics, eye drops, and insulin often expire sooner-sometimes in 28 days after opening. Never use expired medicine, especially for serious conditions like heart disease or seizures. The FDA says expired drugs can lose up to 30% of their potency within a year of expiration. That’s not a small drop-it’s the difference between treatment and no treatment.

Prescription Number and Pharmacy Info
The Rx number is your prescription’s ID. It’s how the pharmacy tracks your refill requests. If you call for a refill and they ask for your Rx number, that’s the one on the label. It’s usually a 6- to 8-digit number. The pharmacy’s name, phone number, and address are right there so you can call with questions. Don’t ignore this. If you’re unsure about your medicine, call them. Pharmacists are trained to explain labels. And the prescriber’s name? That’s your doctor’s name. If you’re ever questioned about the prescription-like at a hospital or by a new pharmacy-you’ll need to know who wrote it.
What the Pill Looks Like
Many labels include a description: "white, round, film-coated tablet" or "clear, colorless liquid." This helps you recognize your medicine if you’re switching bottles or if the label smudges. It’s also how you catch mistakes. If your new bottle says "white tablet" but your old one was blue, something’s wrong. Even if the name matches, the color or shape should match too. The National Drug Code (NDC) is a 10- or 11-digit number that uniquely identifies the drug, manufacturer, and package size. You don’t need to memorize it-but if you’re ever in a hospital or emergency, giving them the NDC helps them verify your meds fast.
Storage Instructions: Keep It Safe
Some meds need to be kept cold. Others need to stay dry. Your label might say "store at room temperature" or "refrigerate." If it says "protect from light," keep it in its original bottle. Don’t transfer pills to a pill organizer if they’re light-sensitive. Some drugs, like insulin or certain antibiotics, lose effectiveness if they get too hot or too cold. Leaving them in a car on a summer day can ruin them. A 2023 USP survey found that 41% of patients store insulin incorrectly-often in the fridge door, where it gets too warm and cold repeatedly.
Warnings: Don’t Skip This Part
This is where the label tells you what could go wrong. It might say "avoid alcohol" or "may cause drowsiness" or "not for use in pregnancy." These aren’t suggestions. They’re safety rules. Some warnings are life-threatening. For example, if you’re on an antibiotic called metronidazole, drinking alcohol can cause vomiting, fast heartbeat, and dangerous blood pressure drops. Other warnings tell you when not to take the drug at all-like if you have liver disease or an allergy. If you see a warning you don’t understand, ask. Don’t assume it doesn’t apply to you.
The Missing Piece: Why You’re Taking It
Here’s the big one: most labels still don’t say why you’re taking the medicine. But they should. A 2020 FDA study found that 78% of patients didn’t know the reason for their prescription. That’s why people take blood pressure pills for headaches, or insulin for diabetes when they don’t have it. The Institute for Safe Medication Practices found that adding the reason-like "for high blood pressure" or "for thyroid condition"-reduces wrong-drug errors by 55%. Some pharmacies now do this voluntarily. If yours doesn’t, ask. You have the right to know why you’re taking something. The USP is pushing to make this mandatory by 2025.
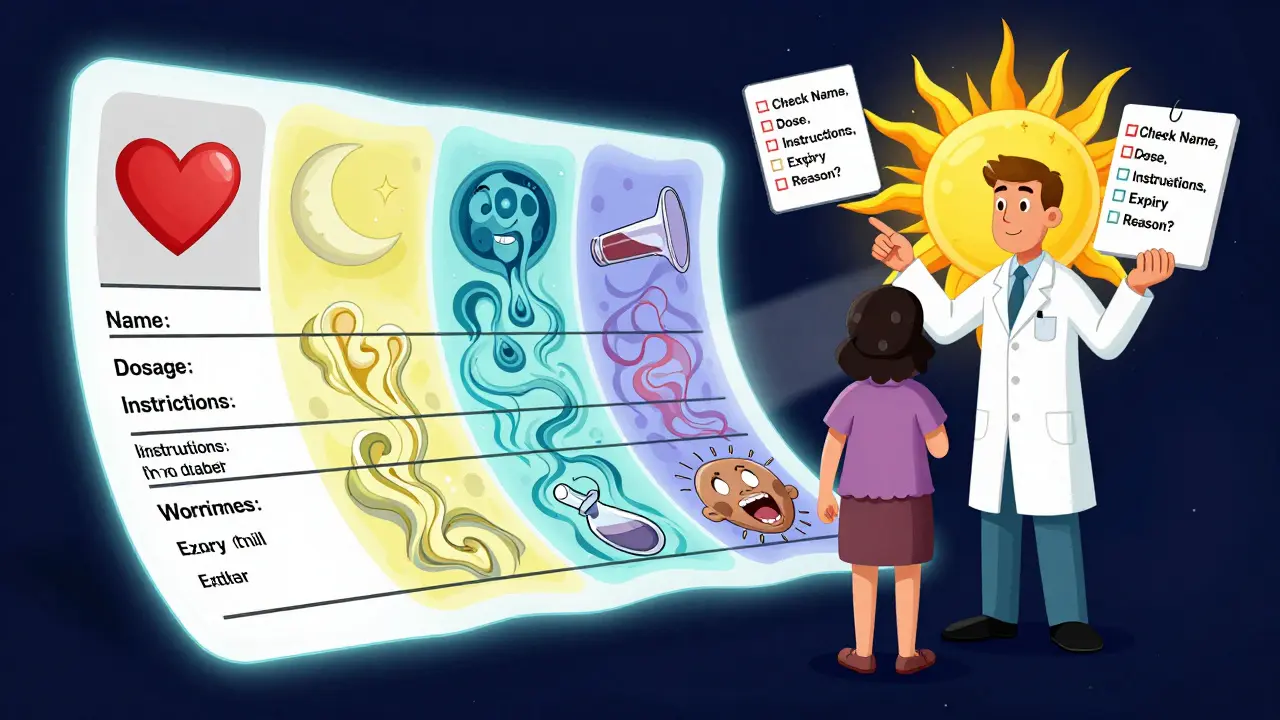
What You Should Do Every Time You Get a New Prescription
Stop. Don’t walk away. Check these five things:
- Your name-is it spelled right?
- Medication name-brand and generic, both match what your doctor told you?
- Dosage-is the strength the same as before? Did it change?
- Instructions-how many times a day? With food? At night?
- Expiration date-is it still good for months, or just a few weeks?
If anything looks off, call the pharmacy before you leave. They’d rather fix it there than have you take the wrong thing.
What to Do If You’re Still Confused
Pharmacists aren’t just there to hand out pills. They’re trained to explain them. Ask them to walk you through the label. Say: "Can you tell me what this is for and how to take it?" Use the "Ask Me 3" method: 1) What is my main problem? 2) What do I need to do? 3) Why is it important? If you’re still unsure, ask them to repeat it back to you. That’s called "teach-back." Studies show it cuts mistakes by nearly 30%.
And if your label doesn’t say why you’re taking the medicine? Ask for a Medication Guide. Some drugs-especially high-risk ones like opioids, blood thinners, or antidepressants-come with a separate printed sheet. That’s your detailed safety guide. If you didn’t get one, ask for it. You’re entitled to it.
Final Tip: Keep a List
Write down every medicine you take-name, dose, why, and how often. Keep it on your phone or in your wallet. Update it every time you get a new prescription. When you see a new doctor, show them the list. It prevents dangerous interactions and helps them catch errors before they happen.
What should I do if my prescription label looks different from last time?
If your label looks different-different color, shape, dosage, or name-don’t assume it’s the same medicine. Call your pharmacy immediately. Sometimes, your insurance switches to a different manufacturer, and the pill looks different even though the active ingredient is the same. But sometimes, it’s a mistake. Always verify. Ask: "Is this the same medicine I got last time?" and "Has the dosage changed?"
Can I take my medication after the expiration date?
It’s not recommended. While some pills may still be safe after expiration, they lose strength over time. For life-saving drugs like epinephrine, insulin, or heart medications, even a small drop in potency can be dangerous. The FDA says expired drugs can be 5% to 30% less effective. For antibiotics, underdosing can lead to resistant infections. When in doubt, throw it out and get a new prescription.
Why doesn’t my label say why I’m taking this medicine?
Many pharmacies still don’t include the reason on the label because their computer systems don’t support it. But that’s changing. The U.S. Pharmacopeia is pushing for this to be required by 2025. In the meantime, always ask your pharmacist or doctor: "Why am I taking this?" Writing it down yourself helps you remember and prevents mistakes.
What’s the difference between a Medication Guide and the label?
The label is what’s stuck on the bottle-it’s short and basic. A Medication Guide is a separate, FDA-approved paper that comes with high-risk drugs. It explains serious side effects, what to watch for, and what to avoid. For example, the Medication Guide for blood thinners like warfarin tells you about bleeding risks and what foods to avoid. You should read it every time you get a refill. If you didn’t get one, ask for it.
Is it safe to use a pill organizer?
Yes, but only if you understand your meds first. Don’t transfer pills into a weekly organizer if they’re light-sensitive, need refrigeration, or come with a Medication Guide. Also, make sure you know the exact name and dose of each pill. A 2023 study found that 37% of pill organizer errors happened because people mixed up similar-looking pills. Always double-check against the original label before transferring.
Nicole Rutherford
December 19, 2025 AT 23:51So many people just grab the bottle and go. I once saw my neighbor take her sister’s blood pressure meds because the pills looked similar. She ended up in the ER. Your name on the label isn’t decoration-it’s your last line of defense.
Don’t be that person.
Chris Clark
December 20, 2025 AT 11:40generic vs brand name trips people up all the time. i got switched from lipitor to atorvastatin and thought they gave me the wrong stuff. called the pharmacy and they laughed and said ‘bro its the same pill’.
learn the generic names. saves money and lives.
William Storrs
December 20, 2025 AT 23:12Hey, you’re doing great just by reading this. Seriously. Most people don’t even look at the label. You’re already ahead of 90% of the population. Keep going. Ask questions. Call your pharmacist. They’re there to help, not just hand you pills.
You got this.
Nina Stacey
December 22, 2025 AT 16:42I used to ignore the expiration date until my mom had a seizure because her anti-seizure med had expired and she thought it was fine because it still looked the same
now i check every bottle like its a bomb and i write the date on the cap with a sharpie and i keep a little notebook on my fridge with every med i take and why and when and i even took a picture of the label on my phone so if i ever lose the bottle i can show someone
its a pain but its worth it because i dont wanna die from being lazy
mary lizardo
December 22, 2025 AT 19:56It is lamentable that the American healthcare system continues to abdicate its responsibility to ensure patient comprehension. The onus should not rest upon the layperson to decipher opaque, poorly formatted labels. The FDA’s failure to standardize mandatory indication fields constitutes a systemic dereliction of duty. One cannot reasonably expect laypersons to be pharmacologists.
jessica .
December 24, 2025 AT 17:03why do they put the expiration date so close? i swear the pharma companies are just trying to make us buy more. i had a 6 month supply of my antidepressant and it expired in 3 months. something fishy going on. they dont want us to save money. its all about profit. the government lets them do this. they control everything.
also why do they make pills so small? are they trying to make us swallow them whole? i think its a mind control thing.
Sajith Shams
December 25, 2025 AT 08:48you people talk about labels like its a mystery. in india we get a printed sheet with the medicine in hindi and english. every pill has the name printed on it. no confusion. why is america so backwards? your pharmacy system is broken. your doctors dont even explain. you need to fix this. stop blaming patients. fix the system.
Erica Vest
December 26, 2025 AT 09:59The NDC code is incredibly useful. I keep a digital spreadsheet of all my meds with the NDC, brand, generic, dosage, and reason. I’ve used it twice when switching pharmacies and once when I had to go to urgent care after a fall. They pulled up my meds instantly. It’s a five-minute setup that saves hours of confusion later.
Highly recommend.
Chris Davidson
December 28, 2025 AT 05:14Expiration dates are a scam. I’ve taken pills two years past their date. Nothing happened. The FDA says they’re safe. Why are you all so scared? Just take the damn pill. You’re not going to die from a 10 mg pill that’s 18 months old.
Stop overthinking.
Glen Arreglo
December 29, 2025 AT 08:44I get that labels are confusing but we gotta meet halfway. I’ve been in the pharmacy biz for 15 years. Most patients just say ‘thanks’ and leave. If you ask ‘what’s this for?’ we’ll explain it till you get it. We’re not robots. We’re humans who want you to be safe.
Don’t be shy. Ask. Seriously.
Matt Davies
December 30, 2025 AT 14:33Pharmacists are the unsung heroes of the healthcare circus. While docs rush in and out, these folks are the ones holding the flashlight in the dark, reading tiny print, and translating gibberish into something you can actually live with.
Next time you’re in, buy them a coffee. Or at least say ‘thank you’ like you mean it.
mark shortus
December 31, 2025 AT 20:52I almost died because of a label mistake. I took my dad’s blood thinner because the bottle looked similar. I didn’t check the name. I woke up in the hospital with a hemorrhage. They said if I’d waited another hour I wouldn’t be here.
Now I take a picture of every label. I have a folder on my phone called ‘DONT TOUCH THIS’. I even have a sticky note on my fridge that says ‘NAME FIRST. ALWAYS.’
If you’re reading this and you’ve never checked your label - stop. Right now. Look. Your life could depend on it.
Takeysha Turnquest
January 1, 2026 AT 15:52Labels are just the surface. The real question is why we’ve outsourced our health to corporations who treat us like inventory. We don’t just need to read the label - we need to dismantle the system that makes reading the label necessary in the first place.
Why should a patient have to become a detective just to not die?
It’s not about ignorance. It’s about power.