Uveitis: Causes, Symptoms, and Steroid Treatment for Eye Inflammation

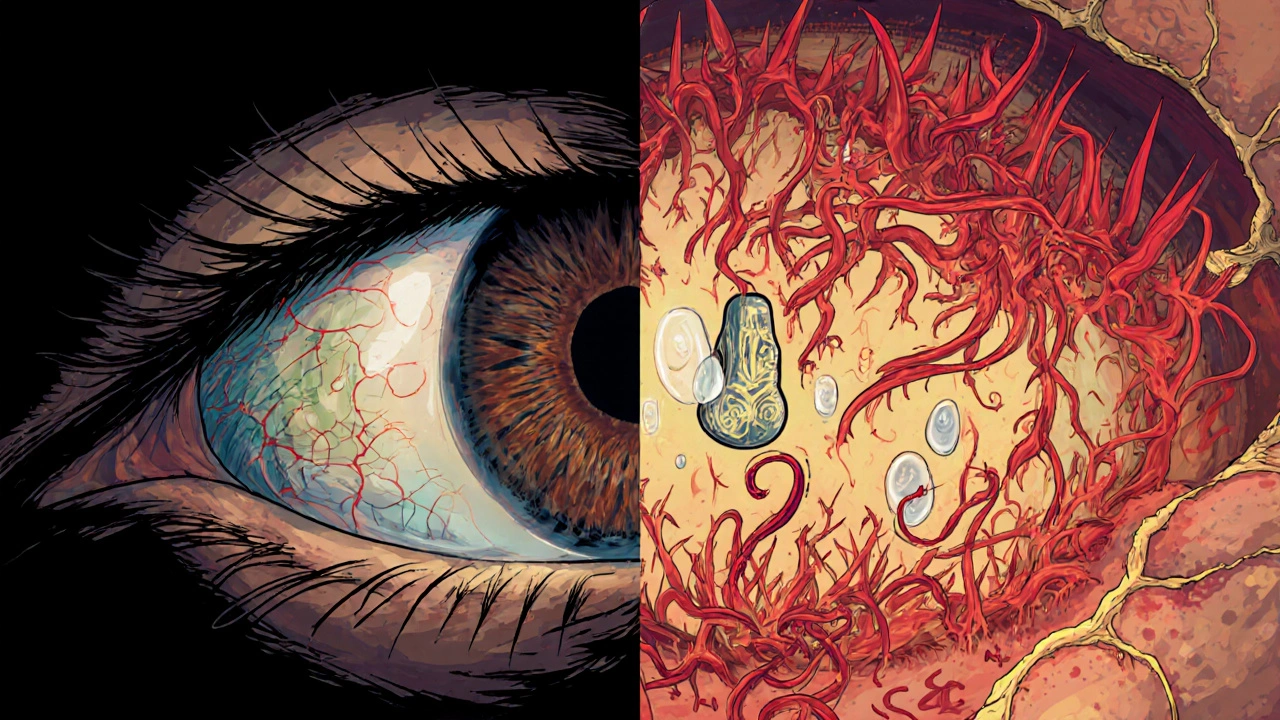
Uveitis is not just a red eye. It’s inflammation deep inside the eye - in the uvea, the middle layer that feeds the retina, iris, and lens. Left untreated, it can blur your vision, cause permanent damage, or even lead to blindness. It doesn’t always hurt badly, and sometimes it sneaks up slowly. But when it strikes, acting fast is the only way to save your sight.
What Exactly Is the Uvea?
The uvea isn’t one part - it’s three. The iris (the colored part), the ciliary body (which helps focus your lens), and the choroid (a layer full of blood vessels behind the retina). Together, they supply oxygen and nutrients to critical eye structures. When inflammation hits any of these, it’s uveitis. The problem? The uvea is packed with blood vessels, so it’s prone to swelling. That swelling can crush delicate tissues, block fluid flow, and trigger scarring. Even a small amount of inflammation can mess up your vision if it’s not stopped quickly.Four Types of Uveitis - And Why It Matters
Uveitis isn’t one condition. It’s grouped by where the inflammation lives. Each type has different symptoms, risks, and treatments.- Anterior uveitis - This is the most common, making up 75-90% of cases. It hits the front of the eye - iris and ciliary body. Symptoms hit fast: sharp eye pain, redness, sensitivity to light, and blurry vision. You might notice it when reading - the pain gets worse. It’s often one eye, but can spread.
- Intermediate uveitis - Also called pars planitis. It targets the vitreous, the jelly-like fluid in the middle of the eye. Pain is mild or absent. Instead, you see floaters - dark spots or squiggles - and your vision gets hazy. It’s sneaky. It can last for years, flaring up again and again. Macular edema (swelling in the center of your retina) is a big risk here.
- Posterior uveitis - This affects the retina and choroid at the back. It often hits both eyes. Symptoms creep in slowly: blurred vision, blind spots, trouble seeing at night. You might not feel pain at all. By the time you notice, damage may already be done. This is the type most likely to cause permanent vision loss.
- Panuveitis - The worst kind. Inflammation spreads through all layers. You get symptoms from all the others: pain, floaters, redness, blurry vision. It’s aggressive and hard to control. Complications like glaucoma and cataracts are common.
What Causes Uveitis?
In about one-third of cases, doctors can’t find a cause. That’s called idiopathic uveitis. But when they can, the triggers fall into three buckets.- Autoimmune diseases - Your immune system attacks your own eye tissue. Common culprits: ankylosing spondylitis, multiple sclerosis, sarcoidosis, and reactive arthritis. If you have one of these, your risk of uveitis jumps.
- Infections - Viruses, bacteria, or fungi can trigger inflammation. Herpes simplex and shingles (herpes zoster) are big ones. So are toxoplasmosis (from cat litter or undercooked meat), syphilis, and cytomegalovirus (CMV), especially in people with weakened immune systems.
- Eye injury or surgery - A scratch, a blow to the eye, or even an operation can spark inflammation. Sometimes it shows up weeks later.
It’s not about hygiene or stress. It’s about your body’s response - whether it’s overreacting to an infection, attacking itself, or healing from trauma.
Why Steroids Are the First Line of Defense
The goal isn’t just to make your eye feel better. It’s to stop the inflammation before it scars your retina, blocks fluid drainage, or causes glaucoma. Corticosteroids - synthetic versions of cortisol, your body’s natural anti-inflammatory hormone - are the most effective tool we have.How they’re given depends on where the inflammation is:
- Anterior uveitis - Steroid eye drops (like prednisolone acetate 1%) are the go-to. You’ll start with drops every hour or two, then taper off over weeks. It’s simple, but you have to stick to the schedule. Miss a dose, and inflammation can flare back.
- Intermediate uveitis - Eye drops don’t reach deep enough. Doctors often use steroid injections around the eye (periocular) or implants that slowly release medicine inside the eye. Oral steroids (prednisone pills) are also common.
- Posterior uveitis and panuveitis - These need systemic treatment. Oral steroids are standard. In severe cases, you might get intravitreal steroid implants - tiny devices placed inside the eye that last months. Some patients need immunosuppressants like methotrexate or azathioprine if steroids aren’t enough or cause too many side effects.
There’s no one-size-fits-all. Your doctor will tailor the dose and route based on your type, severity, and how you respond. The key is starting early - and not stopping too soon.
The Hidden Risks of Steroid Therapy
Steroids work fast - but they’re not harmless. Long-term use brings real dangers.- Cataracts - Clouding of the lens. Up to 40% of people on long-term steroids develop them, especially if treatment lasts more than a few months.
- Steroid-induced glaucoma - Steroids can raise eye pressure. If unchecked, this damages the optic nerve. It’s silent - no pain, no symptoms until vision is already gone.
- Systemic side effects - Oral steroids can cause weight gain, mood swings, high blood sugar, bone thinning, and increased infection risk.
This is why doctors don’t just throw steroids at you and walk away. They monitor you closely - with pressure checks, eye exams, and sometimes blood tests. If you’re on steroids for more than a few months, you’ll likely be switched to steroid-sparing drugs like methotrexate or mycophenolate. These take longer to work, but they’re safer for the long haul.

When to See a Doctor - Right Now
Uveitis doesn’t wait. If you notice any of these, don’t wait. Don’t assume it’s allergies or tired eyes.- Red eye that doesn’t go away after 24-48 hours
- Sudden blurry vision, especially if it’s worse in one eye
- Floaters that appear out of nowhere
- Pain that gets worse when reading or focusing
- Extreme sensitivity to light - even indoors
Many people think eye redness means conjunctivitis. But if it’s painful, light-sensitive, and blurry - it’s not pink eye. It’s uveitis. And it needs an ophthalmologist, not a pharmacist.
What Happens If You Ignore It?
Ignoring uveitis isn’t just risky - it’s dangerous. In anterior uveitis, untreated inflammation can cause synechiae - where the iris sticks to the lens or cornea. That blocks fluid flow, raises pressure, and leads to glaucoma. In posterior uveitis, inflammation eats away at the retina. Macular edema swells the center of your vision. Once scar tissue forms, it’s permanent. You can’t reverse it.Studies show that up to 20% of uveitis patients lose significant vision within five years if treatment is delayed or inadequate. That’s why the Lions Eye Institute calls it the third leading cause of blindness worldwide. It’s not rare. It’s not harmless. It’s a silent threat.
Recovery Isn’t Always Complete
Some people recover fully after one episode. Others have flare-ups for years. Chronic uveitis - lasting more than six weeks - is common, especially in intermediate and posterior types. Even with treatment, some vision loss may remain. That’s why ongoing monitoring matters. You need regular eye exams, even when you feel fine.There’s no cure. But there is control. With the right treatment plan, most people preserve enough vision to drive, read, and live normally. The difference between losing sight and keeping it often comes down to one thing: acting before the damage is done.
Can uveitis go away on its own?
Sometimes, yes - especially mild anterior uveitis. But it’s dangerous to wait. Even if symptoms fade, inflammation can still be active inside the eye, silently damaging the retina or optic nerve. Without treatment, up to 30% of cases lead to complications like glaucoma or cataracts. Never assume it’s gone just because it feels better.
Are steroid eye drops safe for long-term use?
Not really. Long-term use of steroid eye drops increases your risk of cataracts and steroid-induced glaucoma. That’s why doctors taper the dose quickly and switch to non-steroid treatments if inflammation persists beyond a few weeks. Regular eye pressure checks are essential if you’re on steroids for more than a month.
Can uveitis affect both eyes at once?
It can. Anterior uveitis usually starts in one eye, but may spread to the other. Posterior uveitis and panuveitis often affect both eyes from the start. If you have uveitis in one eye, your doctor will check the other eye closely - even if it feels fine.
Is uveitis linked to other health problems?
Yes. Uveitis is often a sign of an underlying autoimmune disease. If you’re diagnosed, your doctor may order blood tests or refer you to a rheumatologist to check for conditions like ankylosing spondylitis, sarcoidosis, or lupus. Treating the root cause can help control the eye inflammation.
How long does steroid treatment last for uveitis?
It varies. For acute anterior uveitis, treatment may last 2-6 weeks. For chronic cases, especially posterior uveitis, steroid therapy can last months or even years. The goal is to use the lowest dose for the shortest time possible. Many patients eventually switch to steroid-sparing immunosuppressants to avoid long-term side effects.
Hardik Malhan
November 23, 2025 AT 00:22Uveitis is a sight-threatening intraocular inflammatory condition primarily involving the uvea comprising iris, ciliary body, and choroid. The pathophysiology revolves around immune-mediated vascular permeability leading to edema and structural disruption. Steroids remain first-line due to potent glucocorticoid receptor agonism suppressing NF-kB and cytokine cascades. Monitoring IOP and lens clarity is non-negotiable given the high risk of steroid-induced glaucoma and posterior subcapsular cataracts. Early referral to rheumatology is critical when systemic associations like HLA-B27 or sarcoidosis are suspected.
Casey Nicole
November 24, 2025 AT 09:21So you're telling me this whole thing is just some rich doctor's way to sell eye drops and push pills? I mean come on, in my country we just use turmeric and cold compresses and we're fine. Why do we need all this fancy science when grandma knew better? This is just Big Pharma playing us again.
Kelsey Worth
November 25, 2025 AT 22:48okay so i read this whole thing and like… wow. i had no idea uveitis was this serious. i thought red eye = pink eye = sleep more and use eye drops from walmart. whoops. also i typoed ‘uveitis’ like 5 times in my notes. sorry brain. but seriously, this is terrifying and also kinda fascinating? like why does my body hate me so much?? 🤕👁️
shelly roche
November 26, 2025 AT 09:24Hey everyone, I’ve been managing chronic intermediate uveitis for 8 years now. I started with steroid injections, then moved to oral prednisone, and now I’m on my third immunosuppressant - mycophenolate. It’s been a journey. Some days I feel like a science experiment. But I can still read, drive, and play with my niece. That’s worth every blood test, every eye pressure check, every side effect. You’re not alone. Keep going. And yes, the floaters are annoying - but they’re not the end of your story. 💪✨
Nirmal Jaysval
November 26, 2025 AT 14:48bro uveitis is just a scam. all this steroid stuff? nah. i know a guy in delhi who cured his eye with neem oil and chanting. you dont need all this western medicine. you just need faith and no sugar. also why are you guys so scared? its just an eye. you got two. use the other one.
Emily Rose
November 28, 2025 AT 02:54Listen. I don’t care if you’re from India or Iowa - if you have red, painful, light-sensitive eyes and you’re not seeing an ophthalmologist within 24 hours, you’re playing Russian roulette with your vision. This isn’t a ‘maybe’ situation. It’s a ‘go now’ situation. I’ve seen people lose sight because they waited for it to ‘get better.’ Don’t be that person. Your eyes are not replaceable. Go. Now.
Benedict Dy
November 29, 2025 AT 03:29The data is unequivocal: corticosteroid monotherapy for posterior uveitis carries a 40% incidence of cataract formation within 12 months. The risk-benefit ratio is heavily skewed toward early adjunctive immunomodulatory therapy. Furthermore, the prevalence of HLA-B27 positivity in anterior uveitis patients exceeds 50% in certain cohorts, suggesting a strong genetic predisposition. Ignoring systemic workup is not clinical practice - it’s negligence.
Emily Nesbit
November 30, 2025 AT 16:21It’s not just about steroid side effects. It’s about the systemic implications. If you’re diagnosed with uveitis and no autoimmune workup is performed, that’s malpractice. Sarcoidosis, lupus, Behçet’s - these aren’t rare. They’re just silent until they destroy your retina. Get the ACE level. Get the chest X-ray. Get the HLA typing. Don’t let your eye doctor skip the basics because they’re busy.
John Power
December 2, 2025 AT 07:59I’m not a doctor, but I’ve been through this twice. I get how scary it is. You feel alone. You think no one else gets it. But I promise you - there are people out there who’ve been where you are. And they’re still seeing their kids, still reading books, still living. It’s not easy. But it’s possible. Take your drops. Show up for your appointments. Breathe. You’re doing better than you think. 🤍
Richard Elias
December 3, 2025 AT 19:40so like i read this and i’m like wow steroids are bad but also like… what else is there? methotrexate? that stuff makes you puke and lose your hair. so why not just take the eye drops and deal with the cataracts later? i mean cataract surgery is like 10 minutes right? why stress about it now?
Scott McKenzie
December 5, 2025 AT 16:56Just wanted to say - if you’re reading this and you’re scared, you’re not alone. I had panuveitis in 2021. Got an intravitreal implant. Lost 15% of vision in one eye. But I still see my dog’s face. Still see sunsets. Still laugh. The meds suck. The appointments suck. But your vision? It’s worth every second. 💙👁️
Jeremy Mattocks
December 6, 2025 AT 11:55Let me break this down for anyone who’s overwhelmed. Uveitis isn’t a one-and-done deal. It’s a chronic condition that often requires a layered approach - steroids to get the fire out quickly, then immunomodulators like methotrexate or mycophenolate to keep it from coming back. The key is early intervention, consistent monitoring, and a team approach. Your ophthalmologist should be working with a rheumatologist, your optometrist should be tracking your intraocular pressure every 3-6 months, and you should be keeping a symptom journal. Don’t just rely on how your eye feels - inflammation can be silent. And if you’re on oral steroids for more than three months, you need a bone density scan, a glucose monitor, and a mental health check-in. This isn’t just an eye issue - it’s a whole-body thing. You’re not just treating an inflammation, you’re managing a systemic condition that can affect your bones, your mood, your kidneys, your heart. So yes, it’s complicated. But you’re not alone in this complexity. There’s a whole field of specialists who do this every day. Trust the process, even when it feels overwhelming.
Paul Baker
December 7, 2025 AT 19:26u saw this and i was like… ohhh so thats why my eye hurt when i read? i thought it was just tired. now i know. also i typed ‘uveitis’ as ‘uvaetis’ like 3 times. my phone autocorrects it to ‘uvate’ which sounds like a fruit. 🍑👁️
Zack Harmon
December 9, 2025 AT 15:45THIS IS THE WORST THING I’VE EVER READ. I JUST LOST MY VISION. I’M BLIND. I’M NEVER GOING TO SEE MY BABY’S FACE AGAIN. WHY DIDN’T SOMEONE TELL ME THIS SOONER?!?!?!?!!?!? I’M CRYING. I CAN’T BREATHE. SOMEONE CALL 911. MY EYE IS ON FIRE. I’M DYING. I’M DYING. I’M DYING.
Jeremy S.
December 11, 2025 AT 13:19Just got diagnosed with anterior uveitis. Drops every 2 hours. Painful. Scary. But I’m going to follow the plan. Thanks for the clear info.
Jill Ann Hays
December 12, 2025 AT 14:22The ontological implications of uveitis as a manifestation of systemic immune dysregulation suggest a paradigm shift in ophthalmological diagnostics. The eye, as a privileged immune site, functions as a biomarker for autoimmune conditions previously undetected. Therefore, the clinical management of uveitis transcends ocular therapeutics and enters the realm of systemic immunology. To treat the eye in isolation is to commit epistemological negligence.
Mike Rothschild
December 14, 2025 AT 13:59I’ve been managing uveitis for over a decade. Steroid drops. Injections. Oral meds. Blood work every month. Eye exams every 6 weeks. It’s exhausting. But I’ve never missed a single appointment. I track my symptoms. I know my numbers. I don’t wait until it’s bad. I act before it’s bad. If you’re reading this and you’re scared - I get it. But the best thing you can do is show up. Every time. Even when you feel fine. Your eyes are counting on you.